Search IMG Library
YOUR SPECIALISM- See all
- Gastroenterology
- Microbiology
- Urology
- Rheumatology
- Stroke Medicine
- Ophthalmology
- Oncology
- Neurology
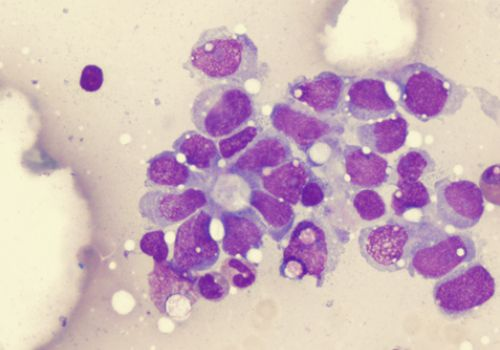
- Histopathology
- Haematology
- ENT Surgery
- Acute Medicine
- Anaesthetics
- Respiratory
- Dermatology
- Geriatrics
- Radiology
- Surgery
- Paediatrics
- Psychiatry
- Emergency Medicine
- Critical Care & ICU
- General Medicine
14 blogs found
- CAREER SUPPORT >
- Career Progression

Specialist Registration and the NHS Histopathology Job Market
For many overseas pathologists, sitting and passing the FRCPath used to be considered the “Golden Ticket” to senior histopathology jobs in the NHS. But is that still the case? And if not, why not? And what does specialist registration, portfolio pathway (CESR) have to do with all of this? First lets have a look at the job market as of 2025 in the NHS, and then we can start to connect the pieces together and give you the best advice to help your application stand out from others.
Histopathology Job Market for IMGs
It may sound surprising in the context of the many pathology vacancies advertised that go unfilled, but there has never been a greater demand for and supply of qualified & experienced histopathologists applying for jobs in the NHS. So why do so many NHS posts remain unfilled?
There is a vacancy rate of between 10 -15% whilst at the same time workload has never been greater. A combination of factors impact this, and senior healthcare leaders have been repeating this same message over the years - people are living longer, people have more complex morbidities, and a growing and developing diagnostic service in the NHS is essential for the NHS to keep up with demand. It is also widely acknowledged that this is coming at a time or decreasing budgets and increasing costs of industry. When we consider this, we start to understand why despite pathology being the backbone of most medical diagnosis, so many NHS histopathology vacancies are not appointed to - despite many candidates applying to their roles.
NHS experience - why is this so important?
Medicine is practiced differently around the world irrespective of the specialty. Whether trained in India, Hong Kong, Singapore, or Nigeria, qualified histopathologists all have something valuable to offer the NHS. Some training programs may lend well to the NHS, and some may take longer to adapt, but generally speaking the consensus is “pathology is pathology”. What does need more time is often the less obvious stuff. New IT systems, new day-to-day language, different reporting expectations, different case referral process etc etc. However, our belief, as a specialist international recruitment company, is that how quickly some adapts is as much down the individual - and good people, open minded professional, quick learners, and motivated pathologist will quickly thrive despite everything being new. Even if it takes a little longer for someone to adjust, ultimately they will adapt and in time become an asset to the United Kingdom’s NHS.
Butfor many NHS Trusts, this is precisely the problem - time is always scarce, as are budgets. And this is why specialist registration and/or NHS experience become so important for them.
GMC Specialist Register - for senior IMGs this means via Portfolio Pathway (CESR)
Specialist Registration with the GMC means that a doctor is recognised as a specialist (or consultant grade) in their field, and can work as a consultant in a permanent NHS role. Essentially it is a certification given by the GMC to show that a doctor has completed a vetted specialist training program a medical specialty, or has demonstrated enough experience equivalent to this. The portfolio pathway (formally known as CESR - but still commonly called as such) is the most common route for doctors who haven’t completed a UK or European training programme to join the GMC Specialist Register. This then allows an overseas-trained doctors to work as a permanent consultant in the NHS.
Specialist registration - how does this affect your job search?
If you’re really not familiar with what specialist registration is, then have a read of this blog before coming back to this article. To understand the content of this blog, and to benefit from our ongoing series discussing portfolio pathways (CESR) applications - you need to be clear on the significance of being on the specialist register, how to compares to the UK CCT training pathways, and the significance of being on the specialist register for your specialty.
In terms of your job search, it is like having or not having NHS experience in some ways. Not being on the specialist register doesn’t necessarily exclude you from being shortlisted for senior or consultant role, but if you have specialist registration - you are all but guaranteed an interview. Histopathology is very much a consultant-led specialty in the UK given the way the training program is structured. People start training and run right through until they’re a consultant, and so most of the histopathology roles in the NHS are consultant positions. If you do not have specialist registration in place, then NHS clients will often look to understand what progress a doctor has made with their CESR portfolio before deciding whether to interview them.
What does this have to do with budgets and finances?
If a trust does not feel they can appoint you substantively (permanently) to a role within 2-years, trusts may often hesitate to appoint. With budgets tight across the NHS, and with high levels of governance over budgets, new recruitment can become so difficult to get approved if it is not seen as sustainable. Vacancy control panels, financial approval, NHS process of advertising and onboarding, often will take so much time from an already time-stressed budget holder that if the appointment is only for 1 or 24-months, and not permanently. Thus, being able to offer some a substantive (permanent) contract is a hugely impactful consideration for NHS pathology departments. If a trust feels that a candidate will complete their CESR in 12 to 24-months - then it becomes a much easier consideration for them.
Can you complete CESR overseas?
Yes and no. You can in theory complete a portfolio overseas, but in reality its very difficult to do and the best thing IMGs can do is to part-complete their applications overseas, before securing a job and completing the process in the UK.
Preparing in advance and organising your portfolio. Make your CV stand out
By organising and getting ahead of our portfolio before coming to the UK - you give yourself an edge over other IMGs making the same applications. A candidate presenting themselves with a full and detailed understanding of what they need to do with their portfolio will stand out a mile compared to others - and will often secure interviews for consultant, specialist or specialty doctor roles in the NHS.
If you want to understand more about the portfolio pathway, the process, or your standing in the histopathology job market then register with us and we can have a quick chat before running through in more detail.

Working as a doctor in Alberta, CA – what IMG’s need to know
Are you an overseas doctor looking for an opportunity to advance your career?
Alberta, Canada might just be your answer! As of recently, Canada is focusing on attracting IMGs, in particular General Practitioners (GPs), consultants and medical specialists, to address staffing shortages and enhance diversity in the profession. Namely, doctors with CCT or CCST qualifications from the UK or Ireland are high in demand. Does this sound like you? With a growing need for healthcare professionals, job opportunities in Alberta come with competitive salaries and excellent potential for career expansion.
With its awe-inspiring scenery and a lifestyle that balances work and play, this province is offering stable and secure jobs for international doctors to join its dynamic healthcare community. This can be where you discover your dream role, but also a take the chance to be part of something bigger—helping to shape the future of healthcare in the province, while enjoying everything Alberta has to offer. And what better place to start your journey than here with us!
In this blog, we’ve put together a clear-cut guide to healthcare in Alberta for overseas doctors. We’ll break down the how’s, the what’s and the who’s; how the healthcare system is structured, who has eligible qualifications and what the licensing processes for UK and Irish-trained doctors are. With this information you can explore potential workplaces and gain an idea of what you can expect in terms of salary. So let’s get you well armed with the most relevant information for you to make the move with confidence.
Here is an overview of Alberta's Healthcare System to help answer any Q’s
Did you know that Alberta’s healthcare system is publicly funded, offering universal coverage to all residents through the Alberta Health Care Insurance Plan (AHCIP)? This means that, regardless of a patient's financial situation, most healthcare services are available at no direct cost at the point of care. Please see here if you’d like to know more about what services are covered, and to what extent, by the AHCIP.
In Alberta, care is provided through a combination of private practitioners, community health centres, hospitals, and long-term care facilities. For GPs, this creates a unique opportunity to foster deeper, more personal connections with patients, as the majority will be covered by AHCIP, allowing for more focused and consistent care.
The system is managed by Alberta Health, which oversees funding, policies, and strategic planning. While AHCIP covers a wide range of services, some, like dental care and prescription medications, might not be fully included, but can typically be supplemented through individual health insurance plans.
How to ensure you are licenced to practice in Alberta, CA.
As an IMG, moving from one healthcare system to another can be a rewarding and sometimes daunting journey, and we’re here to help you navigate the process. First things first you’ll need to ensure you meet the qualifications to practice medicine in the province.
The College of Physicians and Surgeons of Alberta (CPSA) is the regulatory body that ensures all physicians meet the necessary standards.
We’ve highlighted 2 crucial steps to follow to ensure you’re fully prepared:
Assess Your Qualifications. Your first step is to have your medical qualifications recognised in Canada. This involves an assessment by the Medical Council of Canada (MCC), which includes the Medical Council of Canada Evaluating Examination (MCCEE) and a review of your medical school credentials. If your school isn’t on the list of accredited institutions, you may need to complete additional exams, such as the MCCQE Part 1. For a detailed look at these requirements, check out our resource page here.
Applying for Registration with the CPSA. After we’ve helped you through any of the necessary exams, it’s time to apply for registration with the CPSA. There are a few pathways for IMGs:
- Independent Practice: If you meet all the requirements, you can apply for an unrestricted medical license to practice independently.
- Supervised Practice: If you have limited Canadian experience or haven’t completed your residency here, you might need to go through a period of supervised practice, typically lasting one to two years.
- Specialist Registration: If you’re a trained specialist, you’ll need to pass additional exams related to your specialty to obtain a specialist license. We can provide more information on these pathways or write a mini blog explaining them in detail.
Finding Employment Opportunities in Alberta, CA.
Once registered with the CPSA, you can start the exciting part—finding the right job for you! This is where our specialised recruitment consultants will assist you in finding a perfect match. Here are some common practice settings in Alberta:
- Hospitals: From large urban hospitals to smaller rural ones, there are diverse opportunities depending on your specialty.
- Family Medicine: As a family doctor, you’ll often be the first point of contact for patients, especially in rural areas. This is also enabled by many family practices being publicly funded.
- Specialist Care: Alberta has various needs for specialists, making it a great place for IMGs who have completed their specialist training in countries like the UK and Ireland.
- Community Health Centres: These centres focus on serving underserved populations and often seek skilled doctors to join their multi-disciplinary teams.
A simple registration with IMG Connect will kick start your journey of finding the most suitable placement in the perfect setting, matching your needs and goals. Visit here to take the first steps at securing your dream job.
Work Permits and Immigration in Alberta, CA.
As an IMG looking for doctor jobs in Canada, securing a work permit is essential. Alberta’s immigration system is closely linked to federal policies, with many overseas doctors entering Canada through the Express Entry program or other skilled worker pathways. Check the Canadian Government website here for details on your eligibility for Express Entry. Additionally, you may qualify for specific programs aimed at attracting skilled medical professionals, like the Alberta Immigrant Nominee Program (AINP). You can find out more here.
At IMG Connect, we have a secialsed team dedicated to relocating and all the admin that comes with it. Once you have registered with us, you will be put in touch with our relocation specialist to begin discussions on how to gain eligibility to live and work abroad.
What can you expect from life here?
So, what can you expect as you settle into life in Alberta? You’ll be happy to know that this province is known for its cultural diversity and vibrant communities, home to around 4.4 million people. Alberta offers a high standard of living and a great work-life balance, although, like many places, the cost of living can vary—especially in cities like Calgary and Edmonton. But not to worry; competitive salaries for doctors and a wealth of benefits make practicing here worthwhile. Let’s dive into what you can look forward to!
Salaries. Your earnings in Alberta as a doctor can vary depending on your specialty and role. Top-earning physicians can see annual salaries averaging around $440,000, while the overall average for doctors hovers around $280,000. Factors like your working hours and specialty can influence your income, giving you the potential to earn more based on your commitment and expertise. You can see here for a comprehensive breakdown of how your speciality can effect your salary.
Cost of Living and Housing. While Alberta boasts a high quality of life, it's important to consider the cost of living. Cities like Calgary can be pricey when it comes to housing, but smaller towns and rural areas often offer more affordable options. Planning your budget in advance can help ensure a smooth transition, and if you’re working with IMG Connect, we’ll assist you every step of the way!
Cultural Diversity and Community Support. One of the highlights of Alberta is its rich multicultural environment. The province welcomes individuals from around the globe, creating vibrant communities filled with diverse food, festivals, and support networks. As an IMG, you’ll find a welcoming community of fellow medical professionals, and you’ll have the chance to engage with patients from a variety of backgrounds. If you’re curious about the experiences of other IMGs who have successfully made the transition, check out their inspiring stories on our website. Alberta also has a strong support network for IMGs, with professional organizations and programs designed to help you integrate into the Canadian healthcare system. Mentorship opportunities and resources are available through the CPSA and various medical associations.
Work-Life Balance. Alberta’s healthcare system values work-life balance. Your work hours may vary by specialty, but many physicians enjoy flexible scheduling, particularly in community settings. This flexibility is essential, especially if you’re relocating with family and want to maintain a healthy balance between your professional and personal life.
Challenges and Opportunities for IMGs in Alberta, CA
While Alberta offers an abundance of opportunities, it’s essential to be aware of some challenges you may encounter to help secure the job and life that you want.
Challenges
Credential Recognition. Getting your international qualifications recognised can take time. You might need to pass exams, undergo supervised practice, and carefully navigate the regulatory processes.
Cultural Adaptation. Although Alberta is welcoming, adjusting to a new country, culture, and medical system can be a journey. Familiarising yourself with Canadian medical practices and patient expectations is key.
Opportunities
High Demand for Physicians. Alberta’s growing population means there’s a strong demand for healthcare professionals in both urban and rural settings. Being flexible about where you practice can open doors to numerous opportunities, particularly in underserved areas.
Support for IMGs. Alberta’s healthcare system and professional organizations provide various resources for overseas doctors from the UK & Ireland, including orientation programs, mentorship, and, in some cases, financial assistance. And you’re not alone in this journey IMG Connect is here to support you every step of the way.
In a Nutshell
For those who made it this far, you’ll know Alberta is a fantastic place for UK and Irish-trained doctors looking to build a career in Canada. With its strong healthcare system, diverse patient population, and a range of employment opportunities, you’ll find plenty of ways to contribute to healthcare while enjoying life in one of Canada’s most stunning provinces.
While there are challenges to navigate—like licensing and cultural adaptation—the rewards of working in Alberta’s healthcare system are significant. If you’re an IMG ready to practice in Alberta or anywhere in Canada, IMG Connect is excited to help! Our experienced team is here to guide you through every stage of the recruitment process, from licensing to relocation, ensuring you start your journey with confidence and all the tools you’ll need. All that’s left to do now is register with us today to learn more about how we can support your medical career in Alberta!

Working as a doctor in Ontario, CA - What IMGs need to know
Are you an overseas doctor considering a career in Canada?...
..Then look no further! With its stunning landscapes and high quality of life, Ontario is actively seeking international doctors to join its healthcare workforce and invite into its society to help further enhance the medical community. The recent campaign targets IMGs, especially General Practitioners (GPs), consultants, and medical specialists, to address staffing shortages and enhance diversity within the medical profession. Doctors with CCT or CCST qualifications from the UK or Ireland are particularly sought after. With growing demand, doctor jobs in Ontario offer competitive salaries and excellent opportunities for career progression.
Ontario is Canada’s most populous province and home to some of the country’s largest cities, including Toronto, Ottawa, and Hamilton. With its diverse and rapidly growing population, Ontario’s healthcare system offers significant opportunities for IMGs who are interested in pursuing a career in Canadian healthcare.
In this blog, we’ll provide an essential guide to healthcare in Ontario for overseas doctors. We’ll cover the structure of the healthcare system, how to get licensed as a UK or Irish trained doctor, where you might work and what your salary can look like.
To answer some of your q’s - here is an overview of Ontario’s Healthcare System
Did you know that Ontario’s healthcare system is publicly funded and provides universal coverage to all residents through the Ontario Health Insurance Plan (OHIP). This means that, regardless of a patient’s financial status, most healthcare services are free at the point of use. Healthcare in Ontario is delivered by a mix of private practitioners, community health centres, hospitals, and long-term care facilities. For GPs, this presents both an opportunity and a responsibility, as likely most of their patients will be covered by OHIP and will not pay directly for most medical services, which can make way for a more personal and consistent doctor-patient relationship.
Ontario's healthcare system is run by the Ministry of Health and Long-Term Care (MOHLTC), which oversees funding, policies, and planning. While OHIP covers most healthcare services, some services such as dental care or prescription drugs may not be fully covered, but this can be covered by individual health insurance.
How can you work in Ontario as a UK or Irish trained IMG?
For IMGs, entering Ontario’s healthcare system can be a rewarding but slightly complex process. This is where we, at IMG Connect, will be at your service to help guide you through the intricate process. The first step is ensuring that you meet the qualifications required to practice medicine in the province. The College of Physicians and Surgeons of Ontario (CPSO) is the regulatory body responsible for ensuring that all physicians in Ontario meet the necessary standards.
Here’s a step-by-step look at how IMGs can begin their journey to working in Ontario:
1. Assessing Your Qualifications - the first thing you’ll need to do is ensure that your medical qualifications are recognised in Canada. This involves an assessment by The Medical Council of Canada (MCC). The MCC administers the Medical Council of Canada Evaluating Examination (MCCEE) and also assesses your medical school credentials, read more here for a breakdown of the assessments.
If your medical school isn’t on Canada’s list of accredited institutions, you may be required to complete additional exams or qualifications, for example, the Medical Council of Canada Evaluating Examination (MCCQE) Part 1 is often necessary for IMGs to demonstrate that they meet Canadian medical standards. Read more here for a more in depth look at what you might need under your belt as an IMG.
2. Apply for Registration with the CPSO - once you’ve passed the necessary exams, you’ll need to apply for registration with the CPSO. There are three primary pathways for IMGs:
Independent Practice. If you meet all the requirements, you can apply for an unrestricted medical license to practice independently in Ontario.
Supervised Practice. Some IMGs may need to undergo a period of supervised practice (usually for a year or two) before they are granted independent practice rights. This is common for those with limited Canadian experience or who have not completed their residency training in Canada.
Specialist Registration. If you are a trained specialist, you will also need to pass additional exams related to your specialty before being granted a specialist license.
3. Finding employment opportunities in Ontario - once you are registered with the CPSO and raring to go, you can begin the fun part – searching for an ideal opportunity that fits your personal goals, and this is where one of our specialised recruitment consultants can help you find the perfect match. To streamline this process, you can use a comprehensive account-based portal on an MCC web page, called Physicians Apply, to store your medical credentials and other important documents that will be necessary to apply for a doctor job in Canada. When it comes to choosing the right setting to practice in, you have several options available. The most common settings for physicians in Ontario include:
Hospitals - Ontario’s hospitals are diverse, ranging from large teaching hospitals in urban centres to smaller community hospitals in rural areas. Depending on your specialty, you might find opportunities in both public and private hospitals.
Family Medicine – A family doctor is often the primary healthcare provider, especially for patients who live in more rural areas. These settings are used to treat non-emergency medical issues and will often be practicing in a clinic, like a GP surgery, which are often publicly funded.
Specialist care - Ontario has a variety of specialist needs, and many IMGs who have completed specialist training in countries like the UK & Ireland can find work in the province’s various hospitals and clinics.
Community health centres - These centres provide primary care to underserved populations and are often looking for skilled doctors. They are a good option if you want to serve in a multi-disciplinary team and address the needs of specific populations, such as newcomers or low-income individuals.
4. Work permits and immigration – as a Uk or Irish trained doctor, you’ll also need to secure a work permit. Ontario’s immigration system is tied closely to federal immigration policies, and many IMGs enter Canada through the Express Entry program or other pathways that offer skilled workers the chance to become permanent residents. Visit the Canadian Government website here for more details about how to check your eligibility to apply for Express Entry.
As a physician, you may also qualify for specific programs aimed at recruiting skilled medical professionals to Canada. The Ontario Immigrant Nominee Program (OINP) is a popular pathway for skilled workers, including doctors, looking to live and work in Ontario. Find out more here.
What can you expect life to look like in Ontario?
You’ll be pleased to know that Ontario is a culturally diverse province, home to people from all over the world with a healthy population of just over 16 million. Its cities generally offer a high standard of living and excellent work-life balance, however, keeping with current economic trends, the cost of living can be high, particularly in Toronto. This being said, salaries for doctors are very competitive and there are significant benefits to practicing in Ontario. Read on to understand what some of these benefits are.
Salaries – what you earn in Ontario as a doctor can vary, depending on specialisation and what role you are interested in. Top earning doctors in Ontario can see annual salaries of $336,500 on average, where an average salary for a doctor in Ontario can be around $166,000 per anum. There are some ways in which your salary can be affected by your specialisation, for example, the number of hours your role requires you to work, meaning you may have the chance to earn more through longer working hours, or if you are a speci family doctor
Cost of living and Housing - while Ontario offers a high quality of life, it is important to understand the cost of living. Toronto, for example, is one of the most expensive cities in Canada in terms of housing. However, you will see that smaller cities, like Ottawa, Hamilton, or those in more rural Northern Ontario have significantly more affordable options. It's important to plan your housing and lifestyle budget ahead of time to ensure a smooth transition, and if you are taking a role with IMG Connect this is what we will help you to do.
Cultural diversity and Community support - one of the most celebrated things about Ontario is its multiculturalism. The province is home to people from every corner of the world, and this is reflected in the communities, food, festivals, and cultural support networks available. As an IMG, you’ll find a supportive community of fellow medical professionals, and you’ll likely have the opportunity to interact with patients from diverse backgrounds. If you’re interested in learning about some of our previous successful candidates, who’ve forged strong connections in new countries with second languages to master, have a read of some of our IMG Stories available on our website.
Ontario also has a strong IMG community, with many professional networks and organisations aimed at helping you integrate into the Canadian medical system. Programs and mentoring opportunities are often available through the CPSO, medical schools, and other professional groups.
Work-life balance - Ontario’s healthcare system places a significant emphasis on work-life balance. While your work hours can vary depending on your specialty, Ontario offers flexible scheduling for many physicians, especially those working in community settings or clinics. This means you can maintain a balance between your professional responsibilities and personal life, which is crucial if you're relocating with your family.
Challenges and Opportunities for IMGs in Ontario - while Ontario offers numerous opportunities, it’s important to acknowledge some of the challenges that IMGs may face when starting their careers in Canada.
Challenges:
Credential Recognition. The process of getting your international qualifications recognized and gaining the necessary certifications can take time. You may need to pass exams, undergo supervised practice, and navigate the regulatory systems carefully.
Cultural Adaptation. Though Ontario is welcoming, adapting to a new country, culture, and medical system can take time. You’ll need to familiarise yourself with Canadian medical practices, patient expectations, and the specific health needs of Ontarians.
Opportunities:
High Demand for Physicians. Ontario’s population continues to grow, and there is a high demand for medical professionals in both urban and rural areas. If you are flexible about where you practice, you may find numerous opportunities in underserved communities.
Support for IMGs. Ontario’s healthcare system and professional organisations offer various support mechanisms for IMGs, including orientation programs, mentorship, and financial assistance in some cases. You are never alone in this process and, again, this is where IMG Connect will be at your side to support you through the process.
In a nutshell
Ontario offers a wealth of opportunities for UK & Irish trained doctors who are looking for a job in Canada. Ontario is an attractive destination for IMGs who want to contribute to healthcare while experiencing quality of life in one of the world’s most naturally breathtaking and diversely represented provinces. With a strong healthcare system, a diverse patient population, and numerous employment opportunities, we are confident that we can guide you into the perfect role.
While there are challenges to navigate, including licensing requirements and the need for adaptation, the rewards of working in Ontario’s healthcare system are plentiful.
If you’re an IMG looking to practice in Ontario or any other part of Canada, IMG Connect is here and happy to help! Our expertly-trained team is experienced in guiding doctors through every stage of the recruitment process—from licensing to relocation—so you can start your journey with confidence. Reach out today to learn more about how we can support your medical career in Ontario!

Irish Medical Council (IMC) Registration for overseas doctors
To work as a doctor in Ireland you will need to register with the IMC.
The IMC is a public body that maintains the official register of medical practitioners within Ireland and attaining full registration is a multistep process involving a number of different documents. IMG Connect are here to help guide overseas doctors through the various stages of IMC Registration by considering the following topics:
Why do I need IMC Registration?
How much will it cost me?
What are the requirements for IMC Registration?
Recognised IMC qualifications
English language capabilities
Registration and licensing history
ID Check
What is the process?
First, lets understand the types of IMC registration that are available
There are several types of IMC registration that are available, and so understanding the registration type that fits you is really the first step. How do you work this out? Well the IMC website has this very useful eligibility route finder and if you have run this already, we recommend checking through this before starting your application.
You'll see that there are various different divisions of IMC registration, and the full list reads Trainee Specialist Division, Internship Registration, Specialist Division, General Division, Supervised Division and Visiting EEA Practitioners Division. Whilst it might seem a bit confusing we can simplify this for you and say that most IMGs or overseas doctors we are working with will be applying for either the general or specialists division. And what does that mean in practice? Doctors with specialist registration may practise independently, without supervision and may represent themselves as specialists, and anyone with general registration is permitted to practice under certain specifications or supervision. If you have ever looked at GMC registration, its essentially the same.
Ok, and why do I need IMC registration?
Its quite simple really, it is a legal requirement! Practicing medicine in Ireland without IMC registration is illegal, as it is in most countries, so anyone wishing to work in the Irish healthcare system will need to get cracking and ge their IMC registration together.
So how much will IMC registration cost me?
The cost of IMC registration varies depending on the type of registration you are applying for. When looking at the IMC website you might find it quite confusing, as did we initially, but to give an overview we can say the total cost of a new application and granted registration can vary, from roughly €1000 to €1,300 depending on the two main associated considerations and costs below.
Application Fee - there is a non-refundable fee for submitting your application. This fee can vary, so it’s important to check the IMC website for the most current amount here.
Registration Fee - in addition to the application fee, there is the registration fee. Again, this amount depends on what type of registration it is you're applying for i.e. general or specialist.
Whatever the case we recommend budgeting for these costs in advance to avoid any nastyt surprises at the point you are ready to make an application!
Ok - so what are the requirements for IMC registration?
To be eligible for full IMC registration with a license to practice, you’ll need to fulfill the requirements listed below. They are very similar to other medical registrations, think GMC registration for example, and will follow a similar pattern. Essentially, you'll need to show that you have the qualifications and knowledge to work as a doctor, and that you can communicate to the required minimum levels to practice safely in Ireland. Below we have listed out and explained some of the requirement for a successful application with the IMC.
Recognised Primary Medical Qualification - you must have a medical degree from a recognised institution, essentially one that is on the World Directory of Medical Schools. You can easily check by going on their website and finding your medical school. You'll then need to verify this with the EPIC (the online portal managed by the ECFMG) - and you can find some more information on this via our blogs on our website here.
English Language Capabilities - if English is not your first language, you must demonstrate your proficiency through accepted tests such as International English Language Testing System (IELTS) and Occupational English Test (OET). Meeting the IMC’s language requirements is crucial for effective communication in a clinical setting, and they are slightly different to the GMC's scoring requirements for registration. For OET you need 4 B's, and for the IELTS you need to acheive an overall band score of 7.0 and a minimum score of 6.5 in each module. For both OET and IELTS this score mut have been acheived in the last 2-years.
Evidence of Knowledge & Skills - this essentially is the qualification or licensing exam that you are using to register with the Medical Council. This might be a reocgnised overseas postgraduate qualification, an Irish postgraduate qualification, a European Specialist Qualification, or the IMCs licensing exam known as the PRES. Either way, for the majority of docotrs applying they will need to show evidence of something additional
Evidence of Registration and Licensing History - you’ll need to provide information about your previous medical registrations and licenses. This includes a proof of registration document showing that you are registered to practice in your home country or any other country where you have practiced.
Certificates of Good Standing - a Certificate of Good Standing (CGS) is typically required from the medical regulatory authority in your home country. This document confirms that you have no ongoing investigations or disciplinary actions against you and no application will be accepted without these. You'll need to provide a CGS that is dated within the last 3-months, and from every medical regulatory body with whom you've held a registration with in the last 5-years.
What Is the Process?
The process of registering with the IMC involves several steps as below:
Document Preparation - gather all required documents, including your medical degree, transcripts, proof of English proficiency, and certificates of good standing.
Online Application - complete the online application form on the IMC website. Ensure that all information is accurate and complete to avoid delays.
Application Fee Payment - pay the non-refundable application fee when you submit your application.
Submit Supporting Documents - upload all necessary documents through the IMC online portal. Make sure everything is clear and readable.
Await Assessment - after submission, the IMC will assess your application. This process can take several weeks, so patience is key.
Complete Additional Assessments - if required, complete any knowledge and skill tests as specified by the IMC.
ID Check & Receive Registration - once your application is approved, you will receive your IMC registration number and will be invited to attend an ID check. Once this has completed you can then practice medicine in Ireland!
To summarise
Registering with the Irish Medical is a crucial step for any overseas doctors wishing to practice in Ireland. By understanding the requirements and following the outlined process, you can navigate this journey with confidence but we appreciate the process may become difficult or unclear. At IMG Connect we’re here to support you throughout your registration process so if you have any questions or need assistance, don’t hesitate to reach out. Together, we can help you turn your dream of practicing medicine in Ireland into reality!

European Pathologist in the NHS - Digital opportunities & pathways
Recognised qualifications, endless potential
For European-qualified anatomical pathologists, transitioning to the NHS is now smoother than ever. Recognition of specialist qualifications from EEA countries means that most anatomical pathologists can register with the GMC and work as histopathology consultants in the UK. However, it’s not just about recognition; understanding the NHS’s unique approach to pathology can make a significant difference for those making the move.
This series explores the evolution of NHS pathology services, beginning with the Carter Review, which catalysed key changes in UK histopathology. We’ll dive into the practical impact on subspecialisation, digital pathology, and NHS networks, mapping how these changes could shape your NHS experience.
The Carter Review - a catalyst for modernising NHS pathology
In 2008, the UK government commissioned the Carter Review, a significant report aimed at transforming pathology services in the NHS. Led by Lord Carter of Coles, the review highlighted areas for improvement, pushing for efficient, cost-effective, and patient-centred pathology services. For European pathologists joining the NHS, understanding these reforms provides valuable context for today’s NHS setup.
Here’s a look at the key reforms and why they matter:
Centralisation of Pathology Services - centralising pathology services into regional labs, instead of maintaining many smaller units, was one of the Carter Review's foundational recommendations. This shift aimed to reduce duplicate work, improve quality control, and facilitate better investment in advanced equipment for enhanced diagnostic capabilities.
Emphasis on Digital Pathology - digital pathology was a major focus and something most pathologists get excited about! Digital platforms streamline histopathology workflows, enabling faster reporting, reducing storage needs, and allowing for easier peer reviews. The UK is currently one of the most digitally developed pathology systems in Europe—a potential game-changer for those accustomed to more traditional setups.
Standardised Processes and Reporting - the Carter Review recommended standardised protocols to ensure uniformity across NHS services. With a more consistent approach to diagnostics, patients receive equitable care, regardless of which hospital they attend, and what laboratory their biopsy gets sent to. This also aligns with the Royal College’s points-based system which is designed to support system-wide adoption of best practices. You can read more about the RCPath Points based-system here.
Optimising Workforce Efficiency - the review recognized the importance of a balanced, efficient workforce, advocating for an increased role for biomedical scientists (BMS) to relieve histopathologists, allowing them to focus on complex cases. This support system is crucial in reducing diagnostic backlogs and improving patient outcomes.
Building Clinical Networks for Subspecialisation - recognising the benefits of subspecialisation, the review encouraged collaboration across clinical networks. With centralised hubs, referrals to subspecialist pathologists are more efficient, improving access to expert diagnostics, especially for rare or complex cases.
The Modern NHS - so what can a European (EEA) pathologist expect?
In the years following the Carter Review, the NHS has made strides toward a more digital, centralised, and specialised pathology landscape. While some regions are more advanced in implementing these changes, the NHS’s commitment to modernisation is clear. For European pathologists, this means:
A digitalised workspace - NHS laboratories now offer state-of-the-art digital infrastructure, providing opportunities for remote working, enhanced workflows, and digital archiving.
Opportunities for subspecialisation - pathologists can increasingly specialise in one, two, or three specific organ systems or pathology subspecialties, supported by an efficient referral network not just in their laboratory, but in their regional (and national) network.
Job security and flexible working conditions - with high demand and ongoing recruitment needs, NHS consultants enjoy secure employment with the flexibility to work from home as digital systems continue to advance.
Competitive compensation - recent updates to NHS consultant pay scales have increased earning potential, making the NHS an attractive option for European-trained histopathologists. Here you can find the NHS pay circulars, and here we discuss their comparison with other European healthcare systems, focusing on the consultant pay in particular. With pay in the NHS now far higher than many other European countries, its a great moment to take that step upwards into the NHS and UK pathology sector.
Joining the Digital NHS Landscape
If you’re a European pathologist interested in joining the NHS, now is the time to explore your options. The UK welcomes EEA-qualified pathologists to contribute to a healthcare system embracing innovation and collaboration. If you're curious about GMC registration or how your experience could translate to NHS practice, reach out to IMG Connect to discover how you can step into a modernised, supportive, and specialised NHS environment. Alternatively, you can read through our Route to the UK blog for Pathologists blog published on our IMG Library.
Whether you’re ready to make the move or just starting to explore the possibilities, the NHS offers a promising, high salaried, digitally integrated, and patient-centred future for European-trained anatomical pathologists

Working in Jersey’s Private Healthcare
Are you an NHS or overseas-trained doctor looking to boost your main income? You’re not alone! Many doctors employed in the UK turn to the private sector for extra work at some point, and those considering Jersey as a future employer will be pleased to know it is an excellent place to do just that.
With about 30% of Jersey’s population covered by private healthcare insurance, the demand for private services is on the rise. This makes now the perfect time to consider relocating to Jersey, where you can balance public sector responsibilities with exciting opportunities in a growing private healthcare market. Whether you’re looking to enhance your career or simply increase your earnings, Jersey has a lot to offer.
Throughout this blog we will be looking into:
Health and Community Service’s (HCS) Private Patients Services Strategy
Benefits of Working in Jersey’s Private Sector
Career Growth Opportunities for IMGs in Jersey’s Private Healthcare
How to move from NHS to private
Health and Community Service’s (HCS) Private Patients Services Strategy
Since the pandemic, Jersey’s private patient revenues took a hit, but things are looking up. In 2023, private patients contributed £12.2 million to Health & Community Services (HCS), about 5% of its total budget. Now, with the launch of the Private Patients Services Strategy, HCS aims to double that figure to over £24 million.
This growth presents exciting opportunities for consultants and specialists, allowing for enhanced career and skill development alongside the main bulk of their work in public sector.
Having choices in healthcare provision not only brings comfort but can also benefits the entire system. Supporting the option to go private enhances care delivery for both clinicians and patients in Jersey. It’s an exciting time to be part of this evolving landscape!
Jersey’s Private Patients Services Strategy: A Vision for 2024-2028
Jersey has unveiled its Private Patients Services Strategy for 2024-2028, aiming to elevate private healthcare on the island over the next five years. Here’s a snapshot of the key goals:
Attracting Top Talent: The strategy seeks to draw in highly-skilled consultants and specialists from the UK and EEA region, enriching and diversifying Jersey's healthcare expertise.
Expanding Service Options: By broadening the range of private healthcare services, patients will have more tailored choices to meet their specific needs.
Boosting Revenue for Community Benefit: The goal is to double private patient income to over £24 million by 2028, contributing to the overall healthcare system and benefiting all islanders. Think of the potential for your fledgling private practice!
Supporting Healthcare Professionals: The plan emphasises collaboration with doctors. The HCS private patients’ leadership team will work closely with consultants to develop and grow services, backed by government support through stakeholder engagement, giving you the guidance and security to take this big step!
This strategy promises exciting advancements for both healthcare professionals and the community.
Benefits of Working in Jersey’s Private Sector
Thinking about making the switch from public to private healthcare? Here are some compelling reasons:
Career Advancement: The private sector offers numerous opportunities for leadership roles, business partnerships, and even the chance to establish your own practice. For those looking for the next step in their career, this would be great for the portfolio!
Better Work-Life Balance: Generally, Jersey’s healthcare workers report lower burnout rates compared to those in the NHS. This may mean you have more time available to supplement your public sector work, with your private sector work, and not just at the expense of your personal time and sanity!
Support from HCS: The HCS private patients leadership team collaborates with medical consultants to help them develop and enhance commercial services, ensuring mutual benefits for everyone involved.
Government Backing: If you’re interested in the private medical sector, substantial government support is available, whether you want to open your own practice or become a partner, through the
Improving Public Health: By easing the demand for state care, you can help reduce waiting lists, allowing patients to receive timely care and avoid worsening conditions.
Career Growth Opportunities for IMGs in Jersey’s Private Healthcare
Leadership and Business Roles: IMGs can pursue leadership positions, form partnerships, or launch their own practices in Jersey’s expanding private healthcare market.
Specialisation and Niche Services: The opportunity to specialise in areas like cosmetic surgery or oncology allows IMGs to introduce unique treatments and thrive in a patient-focused environment.
Starting a Private Practice: As previously stated, IMGs receive support from Jersey’s Health & Community Services (HCS) for business planning, marketing, and regulations, ensuring a smooth transition to private practice, as well as financial incentives from the government to help start things up.
Networking and Collaboration: Joining a network of specialists offers opportunities for collaboration and knowledge exchange, enhancing career advancement.
Leading Service Expansion: IMGs can take on leadership roles in developing and expanding innovative healthcare services as the sector grows.
Active Role in the Private Patients Strategy: Contributing to Jersey’s Private Patients Services Strategy allows IMGs to help shape the future of private healthcare.
Enhanced Professional Recognition: Working in Jersey’s high-standard private healthcare system helps IMGs build recognition locally and internationally, creating future opportunities worldwide.
How to move from NHS to private in 10 steps
Understand Jersey’s Healthcare System: Jersey has its own independent healthcare system. Consultants often work in private practices or a hybrid model with Jersey General Hospital, where many patients pay for services directly or through insurance.
Research Private Hospitals and Clinics: Key private providers include Lido Medical Centre and Clinique Pinel. Explore opportunities at Jersey General Hospital, which may offer private consulting roles.
Jersey License to Practice: Ensure you’re licensed to practice in Jersey by registering with the Jersey Care Commission, which regulates healthcare professionals on the island.
Private Practice Setup: If starting your own practice, register it with Jersey's Government and secure medical indemnity insurance. Build relationships with private insurers like Bupa and AXA PPP.
Finding Job Opportunities: Jersey has a demand for specialists in fields like orthopaedics and cardiology. Check job listings at Jersey General Hospital and private clinics.
Building a Patient Base: Success in private practice relies on referrals from local GPs and maintaining a strong professional reputation. Consider marketing yourself through websites and local directories.
Work Flexibility: Many consultants work in both public and private sectors. Decide if you want to focus solely on private care or split your time.
Finances and Earnings: Private consultants can earn significantly more than NHS counterparts, but consider Jersey’s higher cost of living when planning your finances.
Housing and Relocation: Understand local housing rules, as competition for rentals can be high. Your employer might assist with relocation.
Legal and Tax Considerations: Familiarise yourself with Jersey’s tax laws, which differ from the UK. Private earnings must be declared to the Jersey tax authorities.
Wrapping Up!
To transition from an NHS role to Jersey private healthcare as a consultant or specialist, you must:
Familiarise yourself with Jersey's healthcare system and private sector.
Obtain the necessary medical licenses and register with the Jersey Care Commission.
Explore employment or business opportunities at private clinics, Jersey General Hospital, or set up your own practice whole researching all opportunities.
Establish a patient base, including networking with local GPs and insurers.
Understand the financial and legal implications of practicing privately in Jersey.

Working in Jersey's Healthcare
Considering a career move to Jersey’s healthcare system? Many UK-trained medical consultants have likely been approached by recruitment agencies regarding job opportunities in Jersey. Whether you’re an IMG doctor, a European-qualified specialist, or an established NHS consultant with a CCT, Jersey might be a career destination that you don’t know much about beyond a few myths and legends. In this article, we’ll explore the key aspects of working as a doctor in Jersey’s healthcare system. Whether you’re an IMG or a UK trainee, we hope to provide you with a clearer perspective on whether Jersey could be an exciting next step in your career.
A Small Island with Big Opportunities!
Whilst not technically being part of the UK, Jersey, the farthest of the Channel Islands from mainland Britain, offers a unique blend of professional opportunities and an enviable lifestyle. It's size may not be impressive, but its healthcare system certainly is. Here’s a snapshot of what you need to know about working in Jersey’s healthcare system, with some notable comparisons to the NHS.
Like most things in Jersey, its healthcare system is robust, well-financed, and highly respected. Whilst still being part of the UK, Jersey operates independently of the NHS, meaning it has its own health service structure, policies, and funding.
Jersey also has a thriving private healthcare sector, with an estimated 30% of the population who have private healthcare insurance, providing another avenue for professionals seeking diverse career opportunities. Working in private healthcare in Jersey allows for a more individualised patient care experience, often with access to state-of-the-art facilities and even more flexibility in clinical practices. Whether in public or private settings, the healthcare landscape here is designed to cater to both professionals and patients.
If you are relocating from the NHS, you may find the transition smooth. Luckily, many of the clinical standards, training, and governance procedures mirror the NHS, so your qualifications will be seamlessly transferable.
Some Key Differences from the NHS:
Smaller Scale, Personal Touch: Jersey’s healthcare system is compact, bringing with it certain advantages. A petit population means fewer patients to manage, so there’s often more time to dedicate to each case, fostering a closer doctor-patient relationship. You’ll be part of a smaller team, which can offer a more personalised, collaborative working environment in Jersey have been expanding compared to larger NHS trusts.
Focus on Mental Health: Mental health services, with a strong focus on community-based care. As a mental health professional, you'll find a commitment to delivering integrated care in both hospital and community settings, providing you with diverse experiences and opportunities for specialisation in your preferred area of practice.
Work-Life Balance: The island’s healthcare system is known for offering a better work-life balance. While NHS roles can often involve long hours and on-call obligations, Jersey’s healthcare professionals frequently report lower levels of burnout. The island’s slower pace of life, along with the stunning beaches and outdoor lifestyle, means you can recharge more effectively during your time off.
Pay and Benefits: Salaries for healthcare professionals in Jersey are competitive and often higher than those offered in mainland UK, as well as other parts of Europe. You can find the Jersey pay scales in full here, whilst we have simplified the pay scales, for your ease, here.
Competitive Tax Rates: And you may’ve heard, but there’s also no VAT in Jersey, which means you can see your earnings go much further. While the cost of living, particularly housing, can be higher, this is often offset by the attractive salary packages and tax rates (a maximum of 20%).
Pensions: When comparing to the NHS’s robust pension schemes, you will see the key differences within the tax environment and contribution rates. This makes Jersey particularly attractive for high-earning specialists or consultants due to the potential to save more into their pensions without hitting the same tax barriers that UK practitioner must adhere to.
Shorter Waiting Lists = More Flexibility: As much as we cherish the NHS, there’s no secret to the pressures it faces day-to-day. Jersey’s healthcare system is not as stretched, where you’ll see waiting times for patients are significantly shorter, and as a clinician you have more flexibility to make important decisions without the same level of resource constraints.
Licensing and Registration
One of the most important steps when making the move is ensuring your qualifications are recognised in Jersey. Most UK-trained doctors and mental health professionals will find this straightforward, but you’ll need to register with the General Medical Council (GMC) or, as a mental health practitioner, the Health and Care Professions Council (HCPC) and obtain a licence to practice in Jersey. The process is akin to the NHS, and guidance is readily available to help you through it on the GMC website.
If you are coming from abroad, the process is similar to what is required for practicing in the UK. You'll need to comply with the following:
Obtain a GMC registration: If you're not already registered, you'll need to meet the GMC's requirements, which may involve providing proof of qualifications, passing relevant exams (such as the PLAB), and demonstrating your English language competence. This process includes psychiatrists, where they will also be required to
Obtain a licence to practice: In addition to being registered, you'll need an active licence to practice. Jersey operates under the same framework, so an active GMC licence is essential.
Visa and work permits: If you're moving from outside the UK or the European Economic Area (EEA), you’ll also need to ensure you have the correct visa and work permits to live and work in Jersey. Employers often assist with this process.
Specialist Registration: As a specialist doctor practicing in Jersey, you will also need to be listed on the GMC's Specialist Register. This requires demonstrating your specialty training, typically through certification of completion of training (CCT) in psychiatry or equivalent qualifications from your home country.
For mental health and care professionals, if you're a psychologist or physiotherapist for example, you would need to register with the relevant UK bodies such as the HCPC, depending on your profession.
Professional Development
The state of Jersey is committed to professional development and getting the most out of its residents, whereby they provide access to a variety of training programmes to enhance your career and opening doors to progression. As previously mentioned, the island has strong ties with UK institutions, and you'll often find that continued professional development follows similar frameworks to the NHS, meaning you won't miss out on growth opportunities!
Perks of the Job
Relocating to Jersey means more than just a new job—it’s a new lifestyle. The island is known for its uniquely stunning landscapes, mild climate and strong sense of community. With its breathtaking beaches, outdoor sports amenities, and short commutes, you’ll enjoy a much calmer, more relaxed pace of life. And with quick travel links to the UK, France and the rest of Europe, you’ll never feel too far from home or adventure. [CS2]
Housing and Relocation Support
It’s worth noting that Jersey has a controlled housing market, and your residential status will determine where you can live. However, many healthcare roles come with relocation support, including assistance with accommodation. Whether you're moving from mainland Britain or further afield, Jersey’s healthcare employers are well known for their generosity with assisted relocation packages, aiming to ensure as smooth
as possible transition.
So, Why Jersey?
Career advancement: Jersey’s healthcare system offers varied and rewarding career opportunities, with less bureaucracy and more flexibility than the NHS.
Competitive salary: Higher wages, lower tax rates, and no VAT make your money go further.
Improved work-life balance: Enjoy shorter commutes, less stress, and a lifestyle focused on health and wellbeing, leaving you full of (Jersey) beans!
Seamless transition: Familiar standards and processes make it easy for NHS and EEA professionals to adapt.
Relocating to Jersey offers the chance to make a real difference. It gives you the exclusive opportunity to progress in a uniquely vibrant healthcare system while enjoying a high quality of life. If you're ready for your next career move, Jersey’s healthcare community is waiting to welcome you!

Career Pathway for a UK Doctor in Training
The NHS offers extensive training schemes and career development for all of its doctors, and such programmes are recognised as a gold standard across the medical world.
Training in the NHS is always in keeping with advances in medical sciences and the progressive landscape of the medical profession, including the more complex ailments of a growing and ageing population. The NHS frequently updates and develops its training programmes, making them attractive to UK graduates and doctors, as well as overseas doctors seeking the very best training.
In this article we will cover the following topics:
The NHS Training Pathway
Graduation to Foundation Training
Specialty Training Programmes
Different types of Specialty Training programmes
Completion of Specialty Training Programme
Should I apply for a training or service post?
As an IMG, can I get onto the specialist register?
How do I secure a service post?
Skip ahead to the relevant section if you know what you're looking for.
The NHS Training Pathway
Many IMGs looking to move to the UK (particularly more junior doctors) will be keen to enter into UK Specialty Training at some point, and as such it is important to understand the UK training pathway from start to finish in order to map your NHS career effectively.
Furthermore, greater understanding of the NHS structure and training offered to doctors in the UK will help an IMG to understand at what grade they can likely enter the system and the salary most appropriate for them.
The NHS Training Pathway describes the journey from medical school to completion of specialist training and is the path most commonly followed by UK trainees.
Graduation to Foundation Training
After graduating from a medical school, doctors gain provisional registration with the GMC allowing them to enter the Foundation Programme - a two-year work-based training programme.
Upon completion of the first year (FY1 or F1) doctors will gain full registration with the GMC and can apply for further study and training in a specialised area – known as Core or Specialty Training, depending on the specialty.
Specialty Training Programmes
Completion of the Foundation Programme allows doctors to apply for Specialty Training in an area of medicine or general practice. There are 60 different specialties to choose from.
A doctor entering year one of Specialty Training is known as an ST1 or CT1 doctor.
Specialty Training programmes can take between three and eight years depending on the specialism chosen.
Doctors can pass through the training quicker depending on how fast they achieve their competencies.
Sometimes doctors do not complete the training pathways in the indicated time for a variety of reasons and it can take between 1 - 4 years longer than indicated in the curricula.
Types of Specialty Training Programmes
There are two different structures for Specialty Training programmes, and these vary between specialties.
Run-through Training Programmes
For these training programmes, you only have to apply once at the beginning of the programme. This is because you are recruited for the full duration of Specialty Training.
These training programme can last from approximately three years for general practice, to five or seven for other specialties such as histopathology.
Uncoupled Specialty Training Programmes
These programmes are split into Core Training and Higher Specialty Training.
Core Training lasts for either two or three years and once complete, allows you to apply for Higher Specialty Training, which can take from three to five years.
Overall, Specialty Training programmes can take anywhere from 5 – 8 years in their entirety, depending on your medical specialty, for example 6 years for psychiatry.
Doctors are known as ST1-3 or CT1-3 during their Core Training and ST4+ level during Higher Specialty Training programmes.
Higher Specialty Training programmes are very competitive, and completion of a UK Core Training programme does not guarantee a Higher Specialty Training post.
Completion of Specialty Training Programme
Upon successful completion of either a run-through or coupled training programme, doctors are awarded a Certificate of Completion of Training (CCT).
At this point doctors are able to make an application for Specialist Registration (or GP Registration) and are able to take up permanent consultant posts.
Training Positions vs Service Posts
As above, competition for places on training programmes within the NHS is very high. As such, we advise that IMGs who are interested in entering core or specialty training in the NHS first obtain a service post for 1 – 2 years.
Following this contract, you can apply for a training post, for which you will be given priority. Not only will this approach give you the best chance of securing excellent training and career progression opportunities in the NHS, it will also give you the chance to settle in to the UK and the NHS system, and help you understand the training post that will suit you the most.
Service posts also offer very competitive rates, so whilst you are getting to know the NHS and settling into life in the UK, you can also ensure that you are financially rewarded.
Specialist Registration for IMGs
IMGs that enter the UK training programmes later on and have not completed the full programme can still get on the specialist register via the CESR-CP route (Certificate of Eligibility for Specialist Registration via a Combined Programme)
Check to see if you're eligible for CESR-CP via the GMC website or read through our detailed blog through our IMG Resources library.
Secure a Trust Doctor Post (with the view to securing a training post at a later date)
You can apply for Trust Doctor or Service Role online via the NHS Jobs website.
However, working with IMG Connect can offer more jobs than are available online with the added benefit of an IMG Consultant speaking directly with services on your behalf to expedite the process and negotiate the best doctor salary for you.
Getting started
Read more useful articles on finding an NHS trust doctor job, training pathways, doctor salaries in the UK, relocation and much more!
Don’t hesitate to get in touch with our team to learn more about the opportunities available to you once as an IMG new to the UK.
For the latest news and updates, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation:
Where do I fit into the NHS with FRCR (Oncology)?
As there is no hard and fast rule for what position you will have after gaining a UK qualification, it is important for IMGs to understand the posts that are available to you after completing FRCR (Oncology).
FRCR (Oncology) is a highly beneficial qualification to achieve, but it does not guarantee you a consultant position in the NHS.
This can be a confusing area for overseas clinical and radiation oncologists, but this blog aims to de-mystify the subject. This article will explain the following topics:
What is FRCR (Oncology) and how does it fit into the UK training programme?
What grade will IMGs, new to the NHS, be offered with FRCR (Oncology)?
Can I take a permanent consultant post if I have FRCR (Oncology)?
CESR opportunities for clinical oncologists in the NHS
Skip ahead to the relevant section if you know what you’re looking for.
FRCR (Oncology) within the UK Oncology Training Programme
Fellowship of the Royal College of Radiologists (Oncology) or FRCR (Oncology) is the postgraduate qualification awarded by the Royal College of Radiologists, the body responsible for the specialties of clinical oncology and clinical radiology throughout the UK.
FRCR (Oncology) is a three-part exam which is a necessary part of the training programme of clinical oncologists in the UK.
For trainees who have chosen to pursue clinical oncology, FRCR (Oncology) Part 1 or CO1 must be passed by the end of ST4.
Clinical oncology trainees will then sit Final FRCR (Oncology), also known as Part 2A and 2B or CO2A and CO2B, usually from ST6 to ST7.
These final exams are important in that they assess a trainee’s knowledge and skills related to the investigation of malignant disease and the care and management of patients with cancer.
Any UK-trained clinical oncologist applying for a CCT in order to work as a substantive consultant must have completed full FRCR (Oncology).
As shown above, UK trainees will also have completed MRCP (UK), although this is not required for overseas clinical oncologists.
Positions for Doctors new to the NHS with FRCR (Oncology)
As an IMG with full FRCR (Oncology), you will be eligible for consultant grade positions in the UK.
You are not guaranteed a consultant position, particularly if you do not have previous consultant position in your home country, but you will certainly be able to attain more senior positions in the NHS, such as a specialty doctor (SAS) or specialist grade.
Consultant positions are the most senior in the UK, and thus the highest paid position for doctors within the NHS pay system.
For further information on how NHS pay scales work for consultants, please see our detailed article here.
Of course, this is assuming that you have also completed the other necessary components to make you eligible for GMC registration.
Alongside your postgraduate qualification, you will need to have passed an English Language Test (either IELTS or OET).
Additionally, you must obtain a Certificate of Good Standing, and submit this to the GMC. Upon the receipt of these three components, you will receive full GMC registration.
Permanent Consultant Posts with FRCR (Oncology)
To take up a permanent consultant position in the NHS, you would need to have Specialist Registration. Specialist Registration (more specifically CESR for most overseas doctors) allows you to take up permanent or substantive consultant roles in the NHS.
The type of consultant position you would be eligible for with FRCR (Oncology) is a locum consultant post.
Firstly, we should clarify the meaning of the term ‘locum consultant’ in the UK. The NHS has two types of locums - Trust locums and Agency locums.
If you are an IMG with full registration, but you are not on the Specialist Register, you are only able to take on consultant positions as a trust locum, but no permanent positions.
Trust locums are hired on a fixed-term contract and are able to better acclimatize themselves to the NHS system, whilst receiving the support and guidance to work towards consultant positions and CESR.
Please note, you can only work as an agency locum if you have a British passport.
CESR Opportunities in the NHS
CESR or the Certificate of Eligibility for Specialist Registration is a route of entry to the Specialist Register for those doctors who have not followed a GMC-approved training programme.
You can read more about CESR in Clinical Oncology through our IMG Resources library here.
IMG Connect are able to help you to secure senior roles such as specialty doctor (SAS), specialist grade or locum consultant in Trusts that offer CESR support.
In these roles, you will have better pay and responsibilities that are more appropriate to your level of experience compared to a trainee. These Trusts have a lot of experience in supporting overseas doctors to progress their careers through CESR.
You can collect evidence of your competences, particularly those specific to the UK Clinical Oncology curriculum and those you may not be able to achieve outside the UK.
These positions also facilitate a faster route to the UK than applying directly through the CESR route, which can take a substantial amount of time.
Get in touch with us to find out more about senior positions in the NHS with CESR support.
Getting started
We hope this blog has been helpful in clarifying your questions about securing senior posts in the NHS with FRCR (Oncology). If you have any further questions regarding the postgraduate exams, CESR or Oncology in the NHS - feel free to contact us directly.
Join the IMG Oncologists Facebook group for access to a community of like-minded clinical and radiation oncologists and dedicated oncology recruiters.
In this group you will find tailored support for oncology IMGs, including access to our NHS and CESR webinars, completely free to all doctors.
You can access our IMG Oncologists community here.
Follow us on social media through the links below for regular news and updates on the Royal College, relocating to the UK and working in the NHS.

CESR - a comprehensive guide for psychiatrists
IMGs from any country in the world can apply for Specialist Registration, provided certain eligibility criteria are met, though there are different routes available based on a doctor’s qualifications and training.
Here we explore specialist registration in psychiatry for overseas consultant psychiatrists and specialists more closely. We’ll cover the Certificate of Eligibility for Specialist Registration (CESR) in more detail, including the application process, costs, and eligibility criteria, along with some other topics, summarised in the headings below:
What is Specialist Registration?
What route to Specialist Registration is best for me as an overseas psychiatrist?
Do I have to complete CESR before I can work in the UK?
Do I need MRCPsych for Specialist Registration?
What is the CESR equivalence process?
What evidence do I need to submit for a CESR in psychiatry?
How much does CESR cost?
How long is the CESR application process?
#IMG Tips
How do I get started?
Skip ahead to the relevant section if you know what you’re looking for.
Specialist Registration
Specialist registration in any specialty means that you can be appointed to a substantive (permanent) consultant position in the NHS. All psychiatrists who wish to take permanent consultant roles in the UK must show evidence of skills, knowledge, and experience in order to apply for Specialist Registration.
For psychiatrists, attaining specialist registration will mean you are qualified to practice independently as a consultant in the NHS.
Specialist Registration is additional to full registration with the GMC and is therefore not required to practice as a psychiatrist in the UK.
Routes to Specialist Registration
There are three types of certificates issued by the GMC for specialist registration, and the type of certificate you receive depends on which training route you followed.
For overseas doctors who have completed their full training outside a GMC-approved training programme, CESR is the route they will usually take towards attaining specialist registration. This route does not require further training, rather the submission of an application.
Doctors who have trained outside the UK or Switzerland, but within an EEA country, will be awarded CCT (Certificate of Completion of Training) after a successful specialist registration application. Specialist Certifications from across the EU are deemed as equivalent by the GMC, and therefore a straightforward application can be made. You can read more about this in the Specialist Registration section under your country on the GMC website here.
Psychiatry Positions in the NHS without CESR
It is important to note that you can apply for more senior psychiatry roles such as a specialty doctor (SAS), specialist grade or a locum consultant without being on the Specialist Register.
Similarly, overseas doctors do not require CESR before moving to the UK to work in the NHS.
In these NHS roles, you will have better pay and responsibilities that are more appropriate to your level of experience compared to a trainee. While working in these positions, you can collect evidence of your competences, particularly those specific to the UK psychiatry curriculum.
These positions also facilitate a faster route to the UK than the CESR route, which can take a substantial amount of time.
MRCPsych for Specialist Registration
Whilst it is always beneficial to complete MRCPsych, overseas doctors looking to join the Specialist Register do not necessarily need to have completed the Royal College postgraduate exams.
The standard test of knowledge in the CCT curriculum is the MRCPsych exam, so passing these exams confirms the attainment of the competencies of the Core Curriculum.
MRCPsych is only a requirement for doctors looking to attain Specialist Registration via the CCT route.
However, if CESR applicants have not successfully completed these exams, they must provide alternative evidence that demonstrates equivalent knowledge to psychiatrists who have passed the MRCPsych exams.
Even if the competencies covered by the exam require something that someone in your position would not routinely undertake (in your sub-specialty for example), you must still provide evidence of it – as the evaluators will not make assumptions outside the evidence presented.
CESR Equivalence Process
Equivalence describes the process of assessing an overseas applicant’s training and experience against the current psychiatry training programme requirements, in order to be awarded CESR.
The equivalence process involves submitting a written body of evidence to the GMC, consisting of:
training and/or competence
skills and knowledge
The Royal College of Psychiatrists will assess each application against the relevant Curriculum before providing a recommendation to the GMC, who will then make a decision.
Please note that Equivalence procedures are the responsibility of the GMC. Applications are made through their Certification Department and initial enquiries should be directed there.
Evidence Requirements for CESR in Psychiatry
Skills & Experience: The evidence provided for a CESR application in psychiatry must cover the knowledge, skills, and qualifications to demonstrate the required competencies in all areas of the General Psychiatry Curriculum, and the Advanced Module in the sub-specialty you are applying in. If evidence is missing from any area of the curriculum, the application will fail.
Primary Evidence: To demonstrate that you can do what is required by the curriculum, you need to submit primary evidence of your clinical practice which shows how you work on a day-to-day basis: letters, reports, assessments etc. References, retrospective case summaries, and reflective notes can all be used in a CESR application, but by themselves they are not sufficient.
Audit and Governance: You are required to submit evidence of your active leadership in audit, including evidence that you have completed at least one audit cycle
Currency of evidence: Your evaluators will be looking for evidence of current competency, generally defined as within the last five years. If you have completed training before this point, it is crucial that you provide evidence of maintaining competency across the whole area of the curriculum.
The GMC asks that only evidence that is strictly relevant is sent as it will help them to process the application quicker. The guidance on compiling your evidence will help you to decide what is relevant and what is not – you can find this on the GMC website here.
As a general guide, the GMC usually expects to see about 800-1200 pages of evidence, divided into four different domains, reflecting those of Good Medical Practice. The GMC recommends that you apportion the evidence provided as shown below:
Domain 1 - Knowledge, skills, and performance
Domain 2 – Safety and quality
Domain 3 – Communication, partnership, and teamwork
Domain 4 – Maintaining trust
Please note, you cannot compensate for evidence lacking in one area by providing more evidence in another area.
The full list of evidence required for each domain can be found on the GMC website here.
The Cost of CESR Applications
All psychiatrists applying for Specialist Registration must pay a fee. For CESR, this fee is £1,676. For CESR-CP and CCT, the cost is £439.
How long does is the application process for CESR in Psychiatry?
The GMC estimate that it can take between six and eight months to receive a decision, from the date you submit your CESR application.
As there is a substantial amount of evidence to gather for a CESR application, the process of preparing all the necessary documentation and applying for CESR can take even longer than this, and a typical candidate will usually set out to complete this within 1 – 3 years.
It is worth noting that more senior psychiatrists, such as consultants, are more likely to have achieved all the competences outlined in the curriculum.
The indicative period of training for a CCT in psychiatry is six years, so it is highly unlikely that you would achieve the competencies required for a CCT in a shorter period of time. Therefore, CESR is not suitable for more junior psychiatrists.
#IMG Tips
Research/think about the types of evidence you will need and begin to gather your evidence well in advance of making your application.
Gather evidence prospectively – this is much easier than retrospectively trying to pull together the evidence under additional pressures.
Make sure that your evidence is of the highest possible quality and is current – you will be assessed against the most recent curriculum.
Ensure that the evidence you collect demonstrates your competence across the whole of the psychiatry curriculum, not just your sub-specialty.
Remember to refer to the most up-to-date Psychiatry CCT Curriculum and Specialty Specific Guidance for the evidence requirements in your specialty.
Create a CESR ‘to-do list’ with sections under the GMC’s 4 domain headings – organise your evidence directly into these sections to manage your progress.
Do not submit original documents – all your copies, other than qualifications you’re getting authenticated must be accompanied by a proformas signed by the person who is attesting to the validity and accuracy of your evidence (your verifier).
Ask an IMG Connect recruitment specialist about NHS psychiatry posts with CESR support. These are not always advertised by a Trust, but we can help you to find a role which aligns well with your career goals in the NHS.
Join the IMG Psychiatrists community – as well as support on Royal College exams, our online community of international psychiatrists and dedicated psychiatry recruiters offers guidance on other aspects of working in the UK, including finding NHS posts and CESR.
Getting started
Many psychiatry IMGs likely haven’t completed a UK-approved training programme, but you could be eligible for Specialist Registration with the GMC via the CESR route. Take a look at our guide to CESR applications for psychiatry for more information on how to apply and what to expect.
If you have any further questions about Specialist Registration, your route to the UK, or would like guidance in finding NHS posts which offer CESR support, please get in touch with us here.
To receive the latest news and updates on all things psychiatry, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.

Specialist Registration (CESR) - what are my options in the NHS?
CESR acts as a route to applying for substantive (permanent) consultant jobs for doctors who have not followed a specialty training programme in the United Kingdom.
In a nutshell it is the option available to doctors practicing as consultants from overseas who wish to gain specialist registration in the UK. Some doctors choose to apply from overseas, others work with IMG Connect to secure a job in the NHS geared at helping them gain entry to the specialist register once in the UK.
If you are working as a consultant in your home country and are eligible for specialist registration in the UK, then as an overseas doctor (IMG) you have a couple of options. Here we focus on applying for CESR from abroad as well as the alternative route, applying for a Specialty Doctor or Fixed Term Consultant job in the UK before applying for CESR with support of your NHS employer.
Both routes lead to gaining CESR and entry to the Specialist Registration, meaning that you can work as a substantive consultant in the NHS. Both take hard work, preparation, evidence gathering, time and dedication. Both options have the same end goal, specialist registration.
It is important to say that no matter how you choose to apply, the CESR process involves submitting a large volume of evidence to demonstrate that you have the equivalent experience, skills and competencies as a doctor who has taken the specialty training route in the UK. Whether applying from overseas or not, some doctors are asked to complete additional experiences to meet this strict standard. Because of this, the process can be lengthy.
Applying for CESR from overseas
This is a great option for Consultants who are not constrained by time and have an understanding department that will support the additional gathering of evidence.
The GMC reckons that it takes between 6 – 9 months between submitting your application and receiving a decision. At IMG Connect our experience tells us that is takes a similar amount of time to gather the evidence prior to submitting. In addition, you must have completed the evidence in the first place in real workplace and clinical scenarios. This can take twice as much time as preparing and submitting. Put simply, the process can be time-consuming and laborious.
Add to this the issue of completing and gathering evidence against the CESR application from overseas. It can prove challenging to ensure that you have completed the full complement of competencies for CESR applications. This can result in the GMC asking for further evidence, adding more time to the process. You may have to identify gaps in your learning and then resolve them. It is not all bad though, this is good practice and will benefit you in the long run.
Applying for a specialty doctor job and/or fixed term consultant post before applying for CESR
For doctors who are keen to secure entry to the Specialist register quickly, and work in the UK as soon as possible, then taking up a Specialty Doctor role with CESR programme, or a Fixed Term Consultant post with CESR programme/support is a good option.
Many NHS hospitals or trusts in the UK will offer access to support, clinical experience and study or preparation time for CESR. This is often built into the weekly job plan, but in some circumstances, this may be arranged informally. Either way, this is a good way for overseas consultants to quickly gather the right evidence for their application with the support of their peers, senior colleagues and NHS employer. This can shorten the time spent on the application overall.
If this sounds like the best option for you, it is wise to start gathering and signing off evidence in your current consultant post. That way you will already have some or most of the required evidence for CESR in place, allowing you to quickly focus on any elements that are missing once in the UK and working in the NHS
Secure a job in the NHS with CESR
Securing a job as a Specialty Doctor with CESR programme, or a job as a Fixed Term Consultant with CESR programme/ support, gives you instant exposure to the UK system, NHS experience and a great start to your career in the NHS.
To discuss whether applying for CESR from overseas or securing a job as a Specialty Doctor or Fixed term consultant with CESR programme is the right route for you towards specialist registration, speak with an IMG Connect consultant, register or send your CV.
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss doctor job options in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.

Specialist Registration - CCT vs CESR vs CESR-CP
Here we take a closer look at the routes available to overseas consultants & experienced doctors who wish to join the GMC’s Specialist Register.
IMGs from any country in the world can apply for Specialist Registration, provided certain eligibility criteria are met, though there are different routes available based on a doctor’s qualifications and training.
To shed some light on the routes to Specialist Registration, we've put together a short article to explain further, including the following topics:
What is Specialist Registration?
What are the different types of Specialist Registration?
Am I eligible?
How do I apply for Specialist Registration and what evidence will I need?
What are the benefits of Specialist Registration?
Are other senior NHS posts available without Specialist Registration?
How much does Specialist Registration cost?
#IMG Tips
Skip ahead to the relevant section if you know what you’re looking for.
Specialist Registration
All doctors who wish to work as permanent consultants in the UK must show evidence of skills, knowledge and experience in order to apply for Specialist Registration. This registration in any specialty means you can be appointed to a substantive consultant post within the NHS.
Specialist Registration is additional to full registration with the GMC.
The 3 Types of Specialist Registration
There are three types of certificates issued by the GMC, and the type of certificate you will receive at the end of your training defines which training route you are on.
The Certificate of Completion of Training (CCT)
The CCT is the route to specialist registration for doctors who have completed a GMC-approved, specialty training programme through the relevant Royal College.
To be eligible for CCT, an applicant’s entire training (including any core years) must have taken place within UK-approved training posts. Please see our blog on career pathways for a UK doctor in training.
The Certificate of Eligibility for Specialist Registration - Combined Programme (CESR (CP))
CESR(CP) is a simplified route for doctors who joined their specialty training programme after ST1, and therefore do not meet the requirement of 4 years duration in GMC-approved training on completion, as they began their training overseas and completed it in the UK.
Doctors on the CESR(CP) route count a combination of approved training and previous experience in non-approved posts (overseas) towards their training time.
The Certificate of Eligibility for Specialist Registration (CESR)
CESR is the route to specialist registration for doctors who have not completed a GMC-approved specialty training programme – doctors who have trained outside of the UK, Switzerland, and the EEA.
These doctors apply directly to the GMC to demonstrate that their specialist training, qualifications, skills, knowledge and experience are equivalent to the requirements for CCT in the UK.
Doctors who have completed their specialist training in the EEA or Switzerland are eligible for direct entry onto the Specialist Register through their Relevant European Qualification (REQ).
For an in-depth guide to CESR, take a look at our blog for overseas doctors here.
Eligibility
Eligibility for Specialist Registration depends on your nationality, qualification and experience.
To meet the minimum eligibility requirements to apply you must have either:
A specialist qualification in the specialty you’re applying in
OR
At least six months continuous specialist training in the specialty you’re applying in
You’ll need to provide evidence of how you’re eligible as part of your application. This could be a copy of your qualification or evidence of your employment.
In your application you must show that you meet the requirements of the CCT curriculum in your specialty.
The CESR certificate is awarded only on the written evidence provided by the applicant. It is not granted on the basis of references or experience.
Applications and Evidence for Specialist Registration
CCT and CESR-CP
Once you have been issued with your Outcome 6 has been issued, you must complete and return the relevant CCT/ CESR(CP) notification to your Royal College along with the following documents:
Copies of any ARCPs that are not on your ePortfolio
ARCPS/evidence of successful progression for any LAT/FTTA/SHO posts counting towards your training (this applies to doctors who were appointed above ST1 only)
You will also need to complete an online GMC form. The link to this form will be emailed to you by the GMC and you should contact your Royal College if you do not receive it.
The GMC has created a guide for each CCT specialty with the relevant royal college or faculty. You can see this here.
CESR
You will need to apply to the GMC, who will then send your application to the Royal College for evaluation. The application process for CESR can be lengthy and potentially stressful, so it is important that you read the GMC’s general guidance and specialty-specific guidance before starting to put together an application.
You will need to provide a portfolio of evidence demonstrating that your specialist training or qualifications are equivalent to the award of a CCT in your specialism in the UK. This information is available for each specialty and Royal College on the GMC website here.
If you apply for an NHS post which provides CESR support, your hospital should assist you in this process.
Once the GMC has sent you a letter informing you that your application is complete and has been sent to your Royal College for assessment, the College is not permitted to discuss your case with you until the GMC has sent you a letter informing you of the decision.
Benefits of Specialist Registration
Specialist registration allows doctors to take up permanent or substantive consultant positions. Without CCT, CESR or CESR-CP, a doctor may only take a Trust locum or fixed-term consultant posts.
Fixed-term and locum posts offer of course offer less stability than permanent consultant posts and require extension.
It is a legal requirement before taking a substantive, honorary or permanent NHS consultant post in the UK that doctors have their names entered on the GMC's Specialist Register.
Senior Positions in the NHS
It is important to note that you can apply for more senior roles such as a specialty doctor (SAS), specialist grade or a locum consultant (locum consultants are not required to be on the Specialist Register).
This way, you will have better pay and roles and responsibilities that are more appropriate to your level of experience compared to a trainee. While working in these jobs you can collect evidence of your competences.
These positions also facilitate a faster route to the UK than the CESR route, which can take a substantial amount of time.
Cost
All doctors applying for Specialist Registration must pay a fee. The fees for 2021 are as follows:
CCT - £439
CESR-CP - £439
CESR - £1,676
#IMG Tips
Research/think about the types of evidence you will need and begin to gather your evidence well in advance of making your application.
Make sure that your evidence is of the highest possible quality and is current – you will be assessed against the most recent curriculum.
Ensure that the evidence you collect demonstrates your competence across the whole of the curriculum, not just your sub-specialty.
Remember to refer to the relevant CCT Curriculum and Specialty Specific Guidance for the evidence requirements in your specialty.
Ask an IMG Connect recruitment specialist about NHS posts with CESR support, these are not always advertised by a Trust, but we can help you to find a role which aligns well with your career goals in the NHS.
Most IMGs likely haven’t completed a UK-approved training programme, but you could be eligible for Specialist Registration with the GMC via the CESR or CESR-CP route. Take a look at our in-depth CESR overview for more information on how to apply and what to expect. If you have any further questions about Specialist Registration, your route to the UK, or would like guidance in finding NHS posts which offer CESR support, please get in touch with us here.
Follow us on social media through the links below for regular news and updates on the Royal Colleges, relocating to the UK and working in the NHS: