Search IMG Library
YOUR SPECIALISM- See all
- Gastroenterology
- Microbiology
- Urology
- Rheumatology
- Stroke Medicine
- Ophthalmology
- Oncology
- Neurology
- Histopathology
- Haematology
- ENT Surgery
- Acute Medicine
- Anaesthetics
- Respiratory
- Dermatology
- Geriatrics
- Radiology
- Surgery
- Paediatrics
- Psychiatry
- Emergency Medicine
- Critical Care & ICU
- General Medicine
11 blogs found
- CAREER SUPPORT >
- Specialty Training

Irish Medical Council (IMC) Registration for overseas doctors
To work as a doctor in Ireland you will need to register with the IMC.
The IMC is a public body that maintains the official register of medical practitioners within Ireland and attaining full registration is a multistep process involving a number of different documents. IMG Connect are here to help guide overseas doctors through the various stages of IMC Registration by considering the following topics:
Why do I need IMC Registration?
How much will it cost me?
What are the requirements for IMC Registration?
Recognised IMC qualifications
English language capabilities
Registration and licensing history
ID Check
What is the process?
First, lets understand the types of IMC registration that are available
There are several types of IMC registration that are available, and so understanding the registration type that fits you is really the first step. How do you work this out? Well the IMC website has this very useful eligibility route finder and if you have run this already, we recommend checking through this before starting your application.
You'll see that there are various different divisions of IMC registration, and the full list reads Trainee Specialist Division, Internship Registration, Specialist Division, General Division, Supervised Division and Visiting EEA Practitioners Division. Whilst it might seem a bit confusing we can simplify this for you and say that most IMGs or overseas doctors we are working with will be applying for either the general or specialists division. And what does that mean in practice? Doctors with specialist registration may practise independently, without supervision and may represent themselves as specialists, and anyone with general registration is permitted to practice under certain specifications or supervision. If you have ever looked at GMC registration, its essentially the same.
Ok, and why do I need IMC registration?
Its quite simple really, it is a legal requirement! Practicing medicine in Ireland without IMC registration is illegal, as it is in most countries, so anyone wishing to work in the Irish healthcare system will need to get cracking and ge their IMC registration together.
So how much will IMC registration cost me?
The cost of IMC registration varies depending on the type of registration you are applying for. When looking at the IMC website you might find it quite confusing, as did we initially, but to give an overview we can say the total cost of a new application and granted registration can vary, from roughly €1000 to €1,300 depending on the two main associated considerations and costs below.
Application Fee - there is a non-refundable fee for submitting your application. This fee can vary, so it’s important to check the IMC website for the most current amount here.
Registration Fee - in addition to the application fee, there is the registration fee. Again, this amount depends on what type of registration it is you're applying for i.e. general or specialist.
Whatever the case we recommend budgeting for these costs in advance to avoid any nastyt surprises at the point you are ready to make an application!
Ok - so what are the requirements for IMC registration?
To be eligible for full IMC registration with a license to practice, you’ll need to fulfill the requirements listed below. They are very similar to other medical registrations, think GMC registration for example, and will follow a similar pattern. Essentially, you'll need to show that you have the qualifications and knowledge to work as a doctor, and that you can communicate to the required minimum levels to practice safely in Ireland. Below we have listed out and explained some of the requirement for a successful application with the IMC.
Recognised Primary Medical Qualification - you must have a medical degree from a recognised institution, essentially one that is on the World Directory of Medical Schools. You can easily check by going on their website and finding your medical school. You'll then need to verify this with the EPIC (the online portal managed by the ECFMG) - and you can find some more information on this via our blogs on our website here.
English Language Capabilities - if English is not your first language, you must demonstrate your proficiency through accepted tests such as International English Language Testing System (IELTS) and Occupational English Test (OET). Meeting the IMC’s language requirements is crucial for effective communication in a clinical setting, and they are slightly different to the GMC's scoring requirements for registration. For OET you need 4 B's, and for the IELTS you need to acheive an overall band score of 7.0 and a minimum score of 6.5 in each module. For both OET and IELTS this score mut have been acheived in the last 2-years.
Evidence of Knowledge & Skills - this essentially is the qualification or licensing exam that you are using to register with the Medical Council. This might be a reocgnised overseas postgraduate qualification, an Irish postgraduate qualification, a European Specialist Qualification, or the IMCs licensing exam known as the PRES. Either way, for the majority of docotrs applying they will need to show evidence of something additional
Evidence of Registration and Licensing History - you’ll need to provide information about your previous medical registrations and licenses. This includes a proof of registration document showing that you are registered to practice in your home country or any other country where you have practiced.
Certificates of Good Standing - a Certificate of Good Standing (CGS) is typically required from the medical regulatory authority in your home country. This document confirms that you have no ongoing investigations or disciplinary actions against you and no application will be accepted without these. You'll need to provide a CGS that is dated within the last 3-months, and from every medical regulatory body with whom you've held a registration with in the last 5-years.
What Is the Process?
The process of registering with the IMC involves several steps as below:
Document Preparation - gather all required documents, including your medical degree, transcripts, proof of English proficiency, and certificates of good standing.
Online Application - complete the online application form on the IMC website. Ensure that all information is accurate and complete to avoid delays.
Application Fee Payment - pay the non-refundable application fee when you submit your application.
Submit Supporting Documents - upload all necessary documents through the IMC online portal. Make sure everything is clear and readable.
Await Assessment - after submission, the IMC will assess your application. This process can take several weeks, so patience is key.
Complete Additional Assessments - if required, complete any knowledge and skill tests as specified by the IMC.
ID Check & Receive Registration - once your application is approved, you will receive your IMC registration number and will be invited to attend an ID check. Once this has completed you can then practice medicine in Ireland!
To summarise
Registering with the Irish Medical is a crucial step for any overseas doctors wishing to practice in Ireland. By understanding the requirements and following the outlined process, you can navigate this journey with confidence but we appreciate the process may become difficult or unclear. At IMG Connect we’re here to support you throughout your registration process so if you have any questions or need assistance, don’t hesitate to reach out. Together, we can help you turn your dream of practicing medicine in Ireland into reality!

Working in Jersey’s Private Healthcare
Are you an NHS or overseas-trained doctor looking to boost your main income? You’re not alone! Many doctors employed in the UK turn to the private sector for extra work at some point, and those considering Jersey as a future employer will be pleased to know it is an excellent place to do just that.
With about 30% of Jersey’s population covered by private healthcare insurance, the demand for private services is on the rise. This makes now the perfect time to consider relocating to Jersey, where you can balance public sector responsibilities with exciting opportunities in a growing private healthcare market. Whether you’re looking to enhance your career or simply increase your earnings, Jersey has a lot to offer.
Throughout this blog we will be looking into:
Health and Community Service’s (HCS) Private Patients Services Strategy
Benefits of Working in Jersey’s Private Sector
Career Growth Opportunities for IMGs in Jersey’s Private Healthcare
How to move from NHS to private
Health and Community Service’s (HCS) Private Patients Services Strategy
Since the pandemic, Jersey’s private patient revenues took a hit, but things are looking up. In 2023, private patients contributed £12.2 million to Health & Community Services (HCS), about 5% of its total budget. Now, with the launch of the Private Patients Services Strategy, HCS aims to double that figure to over £24 million.
This growth presents exciting opportunities for consultants and specialists, allowing for enhanced career and skill development alongside the main bulk of their work in public sector.
Having choices in healthcare provision not only brings comfort but can also benefits the entire system. Supporting the option to go private enhances care delivery for both clinicians and patients in Jersey. It’s an exciting time to be part of this evolving landscape!
Jersey’s Private Patients Services Strategy: A Vision for 2024-2028
Jersey has unveiled its Private Patients Services Strategy for 2024-2028, aiming to elevate private healthcare on the island over the next five years. Here’s a snapshot of the key goals:
Attracting Top Talent: The strategy seeks to draw in highly-skilled consultants and specialists from the UK and EEA region, enriching and diversifying Jersey's healthcare expertise.
Expanding Service Options: By broadening the range of private healthcare services, patients will have more tailored choices to meet their specific needs.
Boosting Revenue for Community Benefit: The goal is to double private patient income to over £24 million by 2028, contributing to the overall healthcare system and benefiting all islanders. Think of the potential for your fledgling private practice!
Supporting Healthcare Professionals: The plan emphasises collaboration with doctors. The HCS private patients’ leadership team will work closely with consultants to develop and grow services, backed by government support through stakeholder engagement, giving you the guidance and security to take this big step!
This strategy promises exciting advancements for both healthcare professionals and the community.
Benefits of Working in Jersey’s Private Sector
Thinking about making the switch from public to private healthcare? Here are some compelling reasons:
Career Advancement: The private sector offers numerous opportunities for leadership roles, business partnerships, and even the chance to establish your own practice. For those looking for the next step in their career, this would be great for the portfolio!
Better Work-Life Balance: Generally, Jersey’s healthcare workers report lower burnout rates compared to those in the NHS. This may mean you have more time available to supplement your public sector work, with your private sector work, and not just at the expense of your personal time and sanity!
Support from HCS: The HCS private patients leadership team collaborates with medical consultants to help them develop and enhance commercial services, ensuring mutual benefits for everyone involved.
Government Backing: If you’re interested in the private medical sector, substantial government support is available, whether you want to open your own practice or become a partner, through the
Improving Public Health: By easing the demand for state care, you can help reduce waiting lists, allowing patients to receive timely care and avoid worsening conditions.
Career Growth Opportunities for IMGs in Jersey’s Private Healthcare
Leadership and Business Roles: IMGs can pursue leadership positions, form partnerships, or launch their own practices in Jersey’s expanding private healthcare market.
Specialisation and Niche Services: The opportunity to specialise in areas like cosmetic surgery or oncology allows IMGs to introduce unique treatments and thrive in a patient-focused environment.
Starting a Private Practice: As previously stated, IMGs receive support from Jersey’s Health & Community Services (HCS) for business planning, marketing, and regulations, ensuring a smooth transition to private practice, as well as financial incentives from the government to help start things up.
Networking and Collaboration: Joining a network of specialists offers opportunities for collaboration and knowledge exchange, enhancing career advancement.
Leading Service Expansion: IMGs can take on leadership roles in developing and expanding innovative healthcare services as the sector grows.
Active Role in the Private Patients Strategy: Contributing to Jersey’s Private Patients Services Strategy allows IMGs to help shape the future of private healthcare.
Enhanced Professional Recognition: Working in Jersey’s high-standard private healthcare system helps IMGs build recognition locally and internationally, creating future opportunities worldwide.
How to move from NHS to private in 10 steps
Understand Jersey’s Healthcare System: Jersey has its own independent healthcare system. Consultants often work in private practices or a hybrid model with Jersey General Hospital, where many patients pay for services directly or through insurance.
Research Private Hospitals and Clinics: Key private providers include Lido Medical Centre and Clinique Pinel. Explore opportunities at Jersey General Hospital, which may offer private consulting roles.
Jersey License to Practice: Ensure you’re licensed to practice in Jersey by registering with the Jersey Care Commission, which regulates healthcare professionals on the island.
Private Practice Setup: If starting your own practice, register it with Jersey's Government and secure medical indemnity insurance. Build relationships with private insurers like Bupa and AXA PPP.
Finding Job Opportunities: Jersey has a demand for specialists in fields like orthopaedics and cardiology. Check job listings at Jersey General Hospital and private clinics.
Building a Patient Base: Success in private practice relies on referrals from local GPs and maintaining a strong professional reputation. Consider marketing yourself through websites and local directories.
Work Flexibility: Many consultants work in both public and private sectors. Decide if you want to focus solely on private care or split your time.
Finances and Earnings: Private consultants can earn significantly more than NHS counterparts, but consider Jersey’s higher cost of living when planning your finances.
Housing and Relocation: Understand local housing rules, as competition for rentals can be high. Your employer might assist with relocation.
Legal and Tax Considerations: Familiarise yourself with Jersey’s tax laws, which differ from the UK. Private earnings must be declared to the Jersey tax authorities.
Wrapping Up!
To transition from an NHS role to Jersey private healthcare as a consultant or specialist, you must:
Familiarise yourself with Jersey's healthcare system and private sector.
Obtain the necessary medical licenses and register with the Jersey Care Commission.
Explore employment or business opportunities at private clinics, Jersey General Hospital, or set up your own practice whole researching all opportunities.
Establish a patient base, including networking with local GPs and insurers.
Understand the financial and legal implications of practicing privately in Jersey.

MSRA – a guide for overseas doctors
Many junior doctors applying for Specialty Training in the UK will need to take the MSRA or Multi-Specialty Recruitment Assessment.
The MSRA plays an important role in the shortlisting and assessment process for entry into postgraduate training in several specialties for ST1 and CT1 level jobs, by assessing essential competencies.
In this blog, we will be taking a closer look at the assessment, focusing on some key questions summarised below:
Who needs to sit the MSRA?
How is the assessment formatted?
What is the structure of the MSRA?
Where can I take the MSRA and how much does the assessment cost?
How can I prepare for the assessment?
#IMG Tips
Skip ahead to the relevant section if you know what you’re looking for.
MSRA Specialties
At present, the MSRA is being used within the following specialties:
ACCS-Emergency Medicine
Anaesthetics
Child and Adolescent Psychiatry
Clinical Radiology
Community Sexual & Reproductive Healthcare
Core Psychiatry Training
Core Surgical Training
General Practice
Neurosurgery
Nuclear Medicine
Obstetrics and Gynaecology
Ophthalmology
Not every specialty uses the MSRA in the same way, however on the whole, candidates’ scores from the MSRA are used as part of CT and ST recruitment to shortlist for interviews and selection centres, as well as making up part of your overall ranking (with the rest coming from interviews selection centres).
For example in 2023, GP, CAMHS, and Core Psychiatry Training will not have any interviews or selection centres and 100% of your rank will be determined by your MSRA scores. Core Surgical Training will also be using the MSRA in shortlisting for the first time this year.
MSRA Format
The MSRA is a single computer-based exam comprising two papers: Professional Dilemmas (PD) and Clinical Problem Solving (CPS). As an exam used across many specialties for entry into Specialty Training, the MSRA assesses a foundation level of competence.
There is an optional five-minute break between the two papers. If candidates choose to take a longer break, the extra time will be subtracted from the time available to complete the CPS paper.
A combination of question types is used within the assessment, primarily extended matching questions (EMQ) and single best answer (SBA) questions, however the assessment may also include multiple best answer (MBA) questions: up to 3 correct answers, picture questions: may include skin lesions, blood reports, ECGs etc., and algorithm questions – drag boxes to the right part of the algorithm or select the correct answer from a list.
Structure of the MSRA
The MSRA last 170 minutes and is divided into two sections: Professional Dilemmas (PD) and Clinical Problem Solving (CPS).
Professional Dilemmas (PD)
The Professional Dilemmas (PD) paper is a Situational Judgement Test (SJT) which measures how a candidate’s judgement regarding challenging professional dilemmas they may face.
The PD paper is not a test of knowledge of problem-solving ability or knowledge specific to specialty training within any specialty, but aims to assess professional attributes which are considered important for successful progression through training and performance in one’s clinical role.
Time: 95 minutes
Number of questions: 50
Context: the PD component is set within the context of Foundation Training with the candidate assuming the role of an F2 doctor. There is also a mixture of settings such as a hospital (across a variety of wards or placements), general practice and out-of-hours clinics.
Core competencies: professional integrity, coping with pressure, empathy and sensitivity (you can find more information on the behavioural indicators linked to these competencies here).
Clinical Problem Solving (CPS)
The Clinical Problem Solving (CPS) paper assesses a candidate’s ability to apply clinical knowledge and make clinical decisions in everyday practice.
Again, the CPS scenarios are based on Foundation level clinical practice. They test a candidate’s ability to synthesise and apply medical knowledge (not just knowledge recall).
Questions may relate to the investigation, diagnosis or management of common and important diseases as well as rare presentations.
Time: 75 minutes
Number of questions: 86
Context: the CPS covers 12 clinical topic areas relevant to general medicine. Each test paper includes a balance of scenarios which cover all 12 topics, including:
Cardiovascular
Dermatology / ENT / Eyes
Endocrinology / Metabolic
Gastroenterology / Nutrition
Infectious disease / Haematology / Immunology / Allergies / Genetics
Musculoskeletal
Paediatrics
Pharmacology and therapeutics
Psychiatry / Neurology
Renal / Urology
Reproductive
Respiratory
Core competencies: investigation, diagnosis, emergency, prescribing, management (you can find more information on these domains here).
Exam Centres for the MSRA
The MSRA is held remotely and is delivered in partnership with Work Psychology Group and Pearson VUE. Candidates will need to register for an account with Pearson VUE and once invited, they can book an assessment at a centre, date and time of your choosing (subject to availability).
The MSRA is delivered globally on several consecutive days in many Pearson VUE Computer Testing Centres. You can find your nearest Pearson VUE assessment centre by visiting the Pearson VUE website.
The exam itself is free to sit, but depending on the centre you choose, there may be additional travel and accommodation costs. It’s therefore advisable to book your seat as soon as possible for the best chance of securing a nearby centre.
Preparation for the MSRA
On the whole, your previous (and current) experience working as a junior doctor will have prepared you for most of the questions and scenarios within the MSRA, although to different extents, depending on where you have gained your experience.
However, as your MSRA scores are often added to the interview score to determine overall rank, or even to exempt you from interview, it may be advantageous to attempt to score as highly as possible.
Blueprint: First and foremost, you should use the MSRA blueprint to better understand the target domains.
Sample questions: Sample questions for both papers are available on the Health Education England Medical Education Hub. You can access these here.
Commercial resources: Exam revision courses, books and online question banks are available, although these are not officially endorsed, and you can find some of the most popular providers below:
Medibuddy
Passtest
eMedica
Passmedicine
4,000 Question bank and mock tests
1,950 Question bank and mock tests
2,200 Question bank and mock tests
2,500 Question bank and mock tests
£30 - £50
£35 - £55
£49 - £119
£25 - £30
#IMG Tips
Start early – Once you have decided to sit the test, plan well in advance to give yourself enough time to prepare and score as highly as possible.
Take a test tutorial – You can take a practice test to familiarise yourself with the controls and screen layouts in advance – see Pearson VUE or Oriel for details.
Negative marking - One mark is given for each correct answer and negative marking is not used within the assessment, so try to answer all questions, even when unsure.
Read carefully - Read the instructions and questions carefully – you may often be looking for the most suitable answer, rather than the only correct one.
Sources
https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/general-practice-gp/how-to-apply-for-gp-specialty-training/what_x0027_s-in-the-msra/structure-of-the-msra
https://medical.hee.nhs.uk/medical-training-recruitment/medical-specialty-training/general-practice-gp/how-to-apply-for-gp-specialty-training/taking-the-msra
https://www.bmj.com/careers/article/a-guide-to-the-multi-specialty-recruitment-assessment-msra-
https://heeoe.hee.nhs.uk/sites/default/files/msra_test_blueprint_information_nov_2019.pdf
The MSRA is a key examination for many IMGs developing their careers by entering Specialty Training. UK training programmes are very competitive and particularly for overseas doctors unfamiliar with the NHS system, taking the time for extensive preparation for the MSRA can greatly impact your chances of being successful in joining a training programme.
Read more useful articles on exams, NHS jobs and salaries in our IMG Resources library.
For regular news and updates, follow IMG Connect on social media using the links below:

Career Pathway for a UK Doctor in Training
The NHS offers extensive training schemes and career development for all of its doctors, and such programmes are recognised as a gold standard across the medical world.
Training in the NHS is always in keeping with advances in medical sciences and the progressive landscape of the medical profession, including the more complex ailments of a growing and ageing population. The NHS frequently updates and develops its training programmes, making them attractive to UK graduates and doctors, as well as overseas doctors seeking the very best training.
In this article we will cover the following topics:
The NHS Training Pathway
Graduation to Foundation Training
Specialty Training Programmes
Different types of Specialty Training programmes
Completion of Specialty Training Programme
Should I apply for a training or service post?
As an IMG, can I get onto the specialist register?
How do I secure a service post?
Skip ahead to the relevant section if you know what you're looking for.
The NHS Training Pathway
Many IMGs looking to move to the UK (particularly more junior doctors) will be keen to enter into UK Specialty Training at some point, and as such it is important to understand the UK training pathway from start to finish in order to map your NHS career effectively.
Furthermore, greater understanding of the NHS structure and training offered to doctors in the UK will help an IMG to understand at what grade they can likely enter the system and the salary most appropriate for them.
The NHS Training Pathway describes the journey from medical school to completion of specialist training and is the path most commonly followed by UK trainees.
Graduation to Foundation Training
After graduating from a medical school, doctors gain provisional registration with the GMC allowing them to enter the Foundation Programme - a two-year work-based training programme.
Upon completion of the first year (FY1 or F1) doctors will gain full registration with the GMC and can apply for further study and training in a specialised area – known as Core or Specialty Training, depending on the specialty.
Specialty Training Programmes
Completion of the Foundation Programme allows doctors to apply for Specialty Training in an area of medicine or general practice. There are 60 different specialties to choose from.
A doctor entering year one of Specialty Training is known as an ST1 or CT1 doctor.
Specialty Training programmes can take between three and eight years depending on the specialism chosen.
Doctors can pass through the training quicker depending on how fast they achieve their competencies.
Sometimes doctors do not complete the training pathways in the indicated time for a variety of reasons and it can take between 1 - 4 years longer than indicated in the curricula.
Types of Specialty Training Programmes
There are two different structures for Specialty Training programmes, and these vary between specialties.
Run-through Training Programmes
For these training programmes, you only have to apply once at the beginning of the programme. This is because you are recruited for the full duration of Specialty Training.
These training programme can last from approximately three years for general practice, to five or seven for other specialties such as histopathology.
Uncoupled Specialty Training Programmes
These programmes are split into Core Training and Higher Specialty Training.
Core Training lasts for either two or three years and once complete, allows you to apply for Higher Specialty Training, which can take from three to five years.
Overall, Specialty Training programmes can take anywhere from 5 – 8 years in their entirety, depending on your medical specialty, for example 6 years for psychiatry.
Doctors are known as ST1-3 or CT1-3 during their Core Training and ST4+ level during Higher Specialty Training programmes.
Higher Specialty Training programmes are very competitive, and completion of a UK Core Training programme does not guarantee a Higher Specialty Training post.
Completion of Specialty Training Programme
Upon successful completion of either a run-through or coupled training programme, doctors are awarded a Certificate of Completion of Training (CCT).
At this point doctors are able to make an application for Specialist Registration (or GP Registration) and are able to take up permanent consultant posts.
Training Positions vs Service Posts
As above, competition for places on training programmes within the NHS is very high. As such, we advise that IMGs who are interested in entering core or specialty training in the NHS first obtain a service post for 1 – 2 years.
Following this contract, you can apply for a training post, for which you will be given priority. Not only will this approach give you the best chance of securing excellent training and career progression opportunities in the NHS, it will also give you the chance to settle in to the UK and the NHS system, and help you understand the training post that will suit you the most.
Service posts also offer very competitive rates, so whilst you are getting to know the NHS and settling into life in the UK, you can also ensure that you are financially rewarded.
Specialist Registration for IMGs
IMGs that enter the UK training programmes later on and have not completed the full programme can still get on the specialist register via the CESR-CP route (Certificate of Eligibility for Specialist Registration via a Combined Programme)
Check to see if you're eligible for CESR-CP via the GMC website or read through our detailed blog through our IMG Resources library.
Secure a Trust Doctor Post (with the view to securing a training post at a later date)
You can apply for Trust Doctor or Service Role online via the NHS Jobs website.
However, working with IMG Connect can offer more jobs than are available online with the added benefit of an IMG Consultant speaking directly with services on your behalf to expedite the process and negotiate the best doctor salary for you.
Getting started
Read more useful articles on finding an NHS trust doctor job, training pathways, doctor salaries in the UK, relocation and much more!
Don’t hesitate to get in touch with our team to learn more about the opportunities available to you once as an IMG new to the UK.
For the latest news and updates, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation:
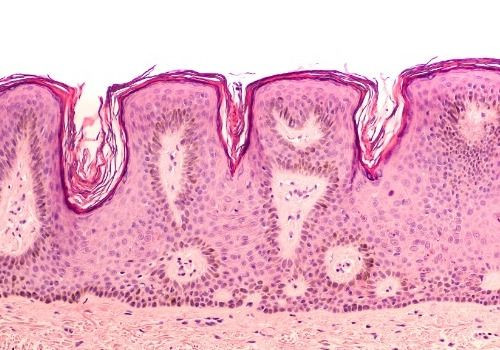
Dermatology SCE – a closer look
The Dermatology SCE is the higher postgraduate qualification provided by the Royal College of Physicians as a specialist qualification for dermatologists. It is one of 11 SCEs offered by the College and offers physicians a higher postgraduate qualification than MRCP which can be used to demonstrate to prospective employers the achievement of a standard equivalent to UK specialist doctors.
Here we take a closer look at the MRCP (UK) Dermatology Specialty Certificate Examination for doctors who have chosen to specialise in dermatology. We cover the content of the exam, as well as fees and the eligibility criteria, which we’ve summarised below with a broad look at the following topics:
What is the SCE in Dermatology?
Where does the SCE fit into my training?
What is the structure of the Dermatology SCE?
How do I apply for the exams and what do they cost?
Where can I sit the exams as an overseas dermatologist?
How should I prepare for the exams as an IMG?
I’ve passed? What’s next?
Skip ahead to the relevant section if you know what you're looking for.
MRCP (UK) SCE in Dermatology
The dermatology specialty certificate exam is administered as a compulsory element of assessment towards the Certificate of Completion of Training (CCT) in dermatology for all UK trainees.
The purpose of an SCE is to:
ensure that certified specialists have sufficient knowledge of their specialty to practice safely and competently as consultants
complement workplace-based assessments
provide a rigorous national assessment to establish public confidence
offer a challenge similar to sub-specialty certification examinations in North America
The SCE as Part of Training in Dermatology
Since the MRCP(UK) exams are taken during the Internal Medicine Training years (ST1-ST3), the dermatology SCE allows physicians to demonstrate that they are able to practice independently at a consultant level.
The SCE has no fixed entry requirements (both for UK and overseas candidates); however, UK trainees would normally sit the SCE in their penultimate year of higher specialty training (ST6). UK trainees should have made at least one attempt at the dermatology SCE by the time of their penultimate year assessment.
For an in-depth guide to the MRCP exams, see our IMG Resources library here.
Exam Structure
The SCE comprises 200 questions which assesses candidates on a wide range of common and important disorders, as set out in the syllabus of the curriculum. This should be taken as an indication of the likely number of questions for each section – the actual number may vary:
Topic
Number of questions
Cutaneous allergy
10
Dermatopathology
10
Dressings & wound care
10
Formulation & systemic therapy
10
General dermatology & dermatology in primary health care
50
Genito-urinary disorders and oral medicine
10
Infectious disease
10
Paediatrics & genetics
30
Photodermatology
10
Psychodermatology
5
Skin biology & research
15
Skin oncology
20
Skin surgery and cosmetic dermatology
10
Total
200
There are two three-hour papers, with the questions in each category distributed across both papers.
All SCEs are computer-based and are administered by Pearson VUE at a test centre in the UK or internationally.
Dermatology SCE Applications
The SCEs are held once a year and all applications are made online through the My MRCP(UK) account, found in the Upcoming Exams section of the Royal College website.
The application process is as follows:
Register online through My MRCP(UK) (candidates have the opportunity at this point to register any special arrangements)
Request a preferred test country and city
Pay applicable examination fee
Application is confirmed via an automatically generated email
Receive test centre confirmation email from Pearson VUE within four weeks of the examination date.
The Royal College of Physicians has created a helpful video guide on SCE applications which you can watch here.
Cost
The cost of the SCE exams are as follows:
UK centres: £665
International centres: £833
Exam Centres
UK Centres
Candidates who choose to sit the dermatology SCE in the UK must contact Pearson VUE to book their test. There are around 137 test centres throughout the UK for each SCE, and the Royal College of Physicians advise that candidates should book their exam as early as possible to secure their preferred test centre, since bookings operate on a first come first served basis.
International Centres
Candidates are given a choice of regions and are then asked to nominate a particular city in that region as their desired test location. The Royal College of Physicians passes this request to Pearson VUE once the application period has closed, and Pearson VUE will confirm final test centre details to candidates via email at least three weeks before the examination date. If the exam is not available in the requested location, candidates will be offered a choice of the nearest available test centres.
Please note, international candidates should not book their own test directly with Pearson VUE - attempting to do so may delay a candidate's application.
The full list of international test centres for the SCE can be found here.
Preparation and Resources for the Dermatology SCE
It can be difficult for IMGs to know where to start with their preparation and revision, particularly as the exam requires a wide breadth of knowledge around the curriculum and should involve reading textbooks, journals and guidelines.
This list should provide a good starting point for any international dermatologists preparing to sit the SCE:
Curriculum - Applicants are tested on a range of common and important disorders in Dermatology as set out in the Joint Royal Colleges of Physicians Training Board’s Specialty Training Curriculum for Dermatology. We recommend getting to know the curriculum as early as possible and using it as a blueprint for your study.
Below are some other good reading materials and sources:
Textbooks
Rook's Textbook of Dermatology - Eds DA Burns, SM Breathnach, N Cox, CE Griffiths
Textbook of Pediatric Dermatology - Eds AD Irvine, PH Hoeger, AC Yan
Dermatology - Eds JL Bolognia, JL Jorizzo, RP Rapini
McKee’s Pathology of the Skin - JE Calonje, T Brenn, A Lazar, P McKee
Journals
British Journal of Dermatology (BJD)
Clinical and Experimental Dermatology (CED)
Journal of the American Academy of Dermatology (JAAD)
Journal of Investigative Dermatology
The Journal of the American Medical Association (JAMA)
Websites
British Association of Dermatologists (BAD)
British Society for Investigative Dermatology (BSID)
British Society for Cutaneous Allergy
British Society for Medical Dermatology
British Society for Dermatological Surgery (BSDS)
DermIS (dermatology image resource)
eMedicine online reference
DermNet NZ (New Zealand dermatology society)
Dermatology e-learning resource
Sample questions: It is a good idea to regularly assess your knowledge and progress using example questions from the current exam syllabus. You can find these here.
For an overview of how to prepare for exams, including advice on study groups, online community support, the best use of online resources & Royal College materials and courses, check out at our blog: IMG Connects Top Tips for exam preparation.
I’ve passed? What’s next?
Congratulations – what an achievement! With your higher postgraduate qualification, you will be able to apply for NHS roles above ST3 which are likely more suited to your seniority and experience – nice one.
Don’t hesitate to get in touch with an IMG medicine recruitment specialist to discuss GMC registration, dermatology positions in the NHS, salaries, suitable UK locations and hospitals for you, and relocation.
To receive the latest news and updates, including the Royal Colleges, GMC registration and the NHS, follow us on social media and join the conversation.
UK Training Pathway for Medical Oncologists
The NHS offers an extensive training scheme and career development for medical oncologists, and the quality of this programme is recognised as a gold standard across the medical community.
The training provided to UK medical oncology trainees is regularly reviewed and updated, in keeping with advances and progression in the landscape of oncology around the world and throughout the profession.
In this article, we will explore the training pathway for medical oncologists in the UK, covering the following topics:
What is the NHS Training Pathway?
How do you enter the training pathway?
What does the specialty training programme look like for medical oncology?
What happens after completing the medical oncology training programme?
Can I enter specialty training in the UK as an IMG?
Skip ahead to the relevant section if you know what you’re looking for.
The NHS Medical Oncology Training Pathway
The NHS training pathway is the name given to the complete programme undertaken by UK trainees, from medical school to the completion of specialist training within i.e. within medical oncology.
It is important for IMGs to understand this as it helps to provide an understanding of at what stage they can most likely enter the system if they are interested in postgraduate training in the UK.
Entering the NHS Training Pathway
After graduating from medical school, doctors with receive provisional registration from the GMC which allows them to enter the Foundation programme (a two-year work-based training programme).
Upon completion of the first year (FY1), doctors will gain full registration with the GMC and will be able to apply for further study and training in a specialised area I.e. medicine – this is known as Internal Medicine Training (IMT), formerly known as Core Training (CT).
Specialty Training in Medical Oncology
The Specialty Training programme in Medical Oncology runs over a 6-year period, and doctors will usually take the indicated time, or slightly longer to complete the Specialty Training programme.
Successful applicants entering into year one of specialty training (ST1), will follow the Joint Royal Colleges of Physicians Training Board 2021 Medical Oncology Curriculum, which sets the expected syllabus as well as required assessments and workload case numbers.
Medical oncology training as an uncoupled programme
As medical oncology is a medicine specialty, aspiring oncology trainees will complete a period of core/ internal medicine training that lasts a period of two years.
This is followed by an open competition to enter a higher specialty training post. It is important to note that the application following core training is competitive and does not guarantee a specialty training post.
Medical oncology higher specialty training will be in total (including OCS) an indicative four-year clinical training programme leading to single accreditation in the specialty. There are no critical progression points during higher specialty medical oncology training, though trainees will be subject to an annual review of progress via the ARCP process and will have to complete all curriculum requirements including passing the medical oncology Specialty Certificate Examination (SCE) prior to obtaining CCT.
Foundation Training (FY1 – FY2)
The foundation programme usually involves six different rotations or placements in medical or surgical specialties. These rotations enable trainees to practise and gain competence in basic clinical skills and forms the bridge between medical school and speciality training.
Selection
Here, trainees will either choose to enter into either Internal Medicine Training or into training to become a general practitioner.
Specialty Training (ST1 – ST6+)
Internal Medicine Stage 1 Training (ST1 – ST2)
In this first stage of the Internal Medicine training programme, trainees develop a solid foundation of professional and generic clinical capabilities, preparing them for participation in acute medicine at a senior level and to manage patients with acute and chronic medical problems in outpatient and inpatient settings. You can find the Curriculum for Internal Medicine Stage 1 Training here.
This will culminate in trainees sitting the MRCP (UK) exams. For more information on the Royal College of Physicians examination suite, take a look at our IMG Resources library here.
Please note, trainees must pass the MRCP examinations prior to beginning Specialty Training in Medical Oncology.
Selection
Here, trainees will either choose to continue with Internal Medicine Training for a further year, to continue with training in a specialty that supports acute hospital care, or to provide primarily out-patient based services in e.g. oncology.
Medical oncology recruitment into ST4 posts usually occurs after 2 years of Internal Medicine Stage 1 training. However, trainees who complete the full three-year IMT programme are also eligible and there is no preferential selection for trainees who have completed either two or three years of training.
Oncology Common Stem (ST3)
The Oncology Common Stem (OCS) has a duration of one year and usually takes place in year 3 of specialty training. Here, the focus is on a trainee’s development of the common oncology capabilities relating to the key areas of overlap between the two specialties (medical and clinical oncology), as well as continuing to develop the generic capabilities expected of all doctors.
Clinical Oncology and Medical Oncology are the two main medical specialities that manage patients with non-haematological malignancy. They often work in partnership with each other, and both offer systemic therapy to patients, but only clinical oncologists administer radiotherapy and there are other differences in work-pattern, approach and focus.
Medical oncologists will have the scientific understanding which underpins radiation-based cancer treatments. During the OCS training year, trainees will gain knowledge of radiotherapy planning and delivery. This will enable them to coordinate the care of cancer patients with the wider multidisciplinary team (MDT), managing patients throughout a treatment pathway.
The curricula for medical and clinical oncology have been aligned to reflect this relationship and include aspects of common training that constitute the Oncology Common Stem (OCS), improving transferability and flexibility for trainees who wish to move between the two specialties.
Please note that medical oncology trainees will not be expected to independently plan or deliver radiation-based cancer treatments.
Medical Oncology Specialty Training & Maintenance of Common Capabilities (ST4 – ST6)
Following successful completion of OCS, medical oncology trainees will complete a subsequent higher specialty-specific programme, this takes place from year 4 – 6. The focus here for trainees is on acquiring medical oncology-specific capabilities, alongside consolidation and further development of the common oncology and generic capabilities.
Trainees will then sit the Medical Oncology Specialty Certificate Examination, usually in the penultimate year of higher specialty training. The globally-recognised exam offers medical oncologists a postgraduate qualification which demonstrates achievement of a standard required of UK specialist trainees.
Please note, the medical oncology SCE is a compulsory component of assessment for the achievement of Certificate of Completion of Training (CCT).
To learn more about the medical oncology SCE, read our detailed blog here.
Completion of the Medical Oncology Specialty Training Programme
Upon completion of the medical oncology training programme, the choice is made whether the trainee will be awarded a Certificate of Completion of Training (CCT) in Medical Oncology. This will be based on high-level learning outcomes – capabilities in practice (CiPs) set out in the curriculum by the Royal College. You can find the 2021 curriculum here.
At this point, medical oncologists are recommended to the GMC for the award of CCT and entry onto the specialist register and can now take permanent consultant posts in the NHS.
Specialist Registration for overseas doctors
Doctors who completed part or all of their medical oncology training outside the UK are eligible for specialist registration through the CESR or CESR-CP pathways. To learn more about specialist registration for overseas doctors, read our blog here.
Joining the Medical Oncology Specialty Training Programme as an IMG
It is possible for overseas doctors to join the Specialty Training programme in Medical Oncology in the UK, however it is very competitive.
IMGs interested in UK specialty training must have:
Full GMC registration
Completion of a minimum 12-month (FY1 equivalent) internship
English language test
PLAB
AND
12 months post-internship experience by the time you begin ST1
Please note, whilst UK trainees are not given priority for specialty training spaces, it can be extremely difficult to join the Specialty Training programme without prior NHS experience.
So here you have it, the NHS Specialty Training pathway for medical oncology trainees in a nutshell. The training programme forms the basis of medical oncology training in the UK, and for overseas oncologists interested in joining the training programme, good knowledge of the pathway allows you to better understand the alignment of your overseas training with the relevant stage of Specialty Training for medical oncology in the UK.
Join the IMG Oncologists Facebook group for access to a community of like-minded oncologists and dedicated oncology recruiters.
In this group you will find tailored resources for oncology IMGs, including access to our MRCP crash courses, completely free to all doctors.
You can access our IMG Oncologists community here.
Follow us on social media through the links below for regular news and updates on the Royal Colleges, relocating to the UK and working in the NHS:
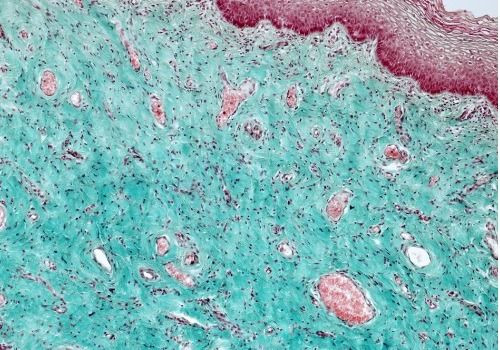
UK Training Pathway for Histopathologists
The NHS offers an extensive training scheme and career development for histopathologists, and the quality and depth of this programme is recognised as a gold standard across the medical community.
The training provided to UK histopathology trainees is regularly reviewed and updated, in keeping with advances and progression in the landscape of pathology around the world and across the profession. This makes the training programme attractive to UK graduates, as well as overseas histopathologists seeking the best training programmes for their field.
In this article, we will explore the training pathway for histopathologists in the UK, covering the following topics:
What is the NHS Training Pathway?
How do you enter the training pathway?
What does the specialty training programme look like for histopathology?
What happens after completing the histopathology training programme?
Can I enter specialty training in the UK as an IMG?
The NHS Training Pathway
The NHS training pathway is the name given to the complete programme undertaken by UK trainees, from medical school to the completion of specialist training within I.e. within histopathology.
It is important for IMGs to understand this as it helps to provide an understanding of at what stage they can most likely enter the system if they are interested in training in the UK.
Entering the NHS Training Pathway
After graduating from medical school, doctors with receive provisional registration from the GMC which allows them to enter the Foundation programme (a two-year work-based training programme).
Upon completion of the first year (FY1), doctors will gain full registration with the GMC and will be able to apply for further study and training in a specialised area I.e. histopathology – this is known as Specialty Training (ST).
Specialty Training in Histopathology
The Specialty Training programme in Histopathology is 5 years long, and whilst doctors may pass through training quicker depending on how quickly they achieve their competencies, this is rarely the case and histopathologist will usually take the indicated time, or slightly longer to complete the Specialty Training programme.
Successful applicants entering into year one of specialty training (ST1), will follow the Royal College of Pathologist’s 2021 Histopathology Curriculum, which sets the expected syllabus as well as required assessments and workload case numbers.
Histopathology training as a run-through programme
Unlike some specialisms where you complete a period of core training before entering into specialty training (requiring two applications), histopathology specialty training works as a run-through programme. You only have to apply once, at the beginning of the programme, as you are recruited for the full duration of Specialty Training.
Foundation Training (FY1 – FY2)
The foundation programme usually involves six different rotations or placements in medical or surgical specialties. These rotations enable trainees to practise and gain competence in basic clinical skills.
Specialty Training (ST1 – ST5+)
ST1)
Year one trainees enter the training programme. In this first stage, trainees will initially develop knowledge of laboratory work, with basic training in all areas of cellular pathology.
Training starts with a 1-2 week induction from the training school. This includes some time in the lab seeing how specimens are prepared and processed. Trainees are taught how to use a microscope, how to approach simple cases under the microscope and the principles of macroscopic assessment and sampling (AKA ‘cut up’). Many training schools do a separate autopsy induction.
When not at block teaching weeks, trainees are rotating through the various specialities in histopathology.
ST2 – ST3
This part of training takes place from year 2 to year 3, with the focus on achieving the FRCPath Part 1 Exam. This will normally be taken after 18 – 24 months of training.
Trainees will consolidate and develop their knowledge base from ST1. Year two trainees are given more independence and are expected to be able to cut up most specimens by the end of this stage.
In many deaneries, this is the time when trainees complete rotations in sub specialities including paediatric pathology, neuropathology and oral pathology. Trainees may rotate to placements in local district general hospitals to gain valuable experience in managing a general histopathology workload.
Autopsy and cervical cytology training continue as mandatory elements of ST2-ST3. Some trainees choose not to continue these specialities when they have completed this stage.
The FRCPath Part 1 exam aims to determine whether you have successfully acquired a core body of knowledge that will underpin your ability to practise in Histopathology.
For more information of the first exam in the Royal College of Pathologists examination suite, take a look at our IMG Resources library here.
Please note, trainees must pass the FRCPath Part 1 examination at the end of ST3 in order to progress to ST4.
Selection
Here, trainees will either choose to continue with general histopathology or peruse subspecialisation in neuropathology, paediatric/perinatal pathology, cytopathology or forensic pathology.
ST3 – ST4
This training takes place from years 3 – 4, where trainees will either continue with general histopathology or peruse subspecialisation in neuropathology, paediatric/perinatal pathology, cytopathology or forensic pathology. Trainees are expected to be competent in the macroscopic and microscopic assessment of all specimens, and will also receive training in leadership, management and teaching in preparation for their future roles as consultants.
The focus during this stage is also on achieving the FRCPath Part 2 Exam, thereby obtaining the status of Fellow of the Royal College of Pathologists.
This final exam is designed to test your practical skills and understanding, and show that you can apply your expertise appropriately and safely.
Trainees who wish to continue in general histopathology may opt to sit further exams in cervical cytopathology and autopsy practice if they wish to continue these as a consultant.
To learn more about the final exam in the in FRCPath examination suite, read our detailed blog here.
Please note, trainees must pass the FRCPath Part 2 examination at the end of ST4 in order to progress to ST5.
ST5+
This is the final stage of training before CCT during which histopathology trainees may wish to peruse special interests in particular subspecialties, such as gastrointestinal, skin or gynaecological pathology. Having passed the FRCPath Part 2 exam, trainees will continue to take on responsibility to enable the transition to independent practice required of those with CCT, i.e. signing out reports without consultant review.
Completion of the Histopathology Specialty Training Programme
Upon completion of the training programme, the choice is made as to whether the trainee will be awarded a Certificate of Completion of Training (CCT) in Histopathology. This will be based on criteria set out in the curriculum by the Royal College. You can find the 2021 curriculum here.
At this point, the histopathologists are entered onto the specialist register and can now take permanent consultant posts in the NHS.
Specialist Registration for overseas doctors
Doctors who completed part or all of their histopathology training outside of the UK are eligible for specialist registration through the CESR or CESR-CP pathways. To learn more about specialist registration for overseas doctors, read our blog here.
Joining the Histopathology Specialty Training Programme as an IMG
It is possible for overseas doctors to join the Specialty Training programme in Histopathology in the UK, however it is very competitive.
IMGs interested in UK specialty training must have:
Full GMC registration
Completion of a minimum 12-month (FY1 equivalent) internship
English language test
PLAB
AND
12 months post-internship experience by the time you begin ST1
Although UK trainees are not given priority for specialty training places, it can be very difficult to join the Specialty Training programme without NHS experience.
So here you have it, the NHS Specialty Training pathway for trainees in a nutshell. This training scheme is the core of training for histopathologists in the UK, and for IMGs looking to join the training programme, understanding of the pathway allows you to better align your overseas training with the relevant stage you would enter into Specialty Training in the UK.
If you have any further questions about your route to the UK as an overseas histopathologist, FRCPath, or any other aspect of GMC Registration, the NHS or the UK, please get in touch with us here.
We'd also like to invite you to join the IMG Histopathologists online community - as well as support on Royal College exams, our Facebook group of international pathologists and dedicated pathology recruiters offers guidance on other aspects of working in the UK, including finding NHS posts and CESR.
Follow us on social media through the links below for regular news and updates on the Royal Colleges, relocating to the UK and working in the NHS:

UK Training Pathway for a Psychiatrist
Training in the NHS offers an extensive training scheme and career development for psychiatrists, with the quality and depth of this programme being recognised as a gold standard throughout the international medical community.
In line with developments and progression in psychiatry across the field and around the world, training provided to UK psychiatry trainees is regularly reviewed and updated. This should make the training programme attractive to UK graduates, as well as IMG psychiatrists seeking the best training programmes for their field and career development.
In this article, we will explore the training pathway for psychiatrists in the UK, with a broad look at the following topics:
What is the NHS Training Pathway?
How do you enter the training pathway?
What does the specialty training programme look like for psychiatry?
What happens after completing the psychiatry training programme?
Can I enter specialty training in the UK as an IMG?
The NHS Training Pathway
The NHS training pathway refers to the complete programme for UK trainees, from foundation training to the completion of specialist or higher training, where candidates may be eligible for a CCT within their chosen specialism, such as General psychiatry or any of its sub-specialties.
It is important for IMGs to understand this process, as it clarifies what stage they can most likely enter the system if they are interested in training in the UK.
Entering the NHS Training Pathway
After graduating from medical school, doctors will receive provisional registration from the GMC which allows them to enter the Foundation programme (a two-year work-based training programme).
Upon completion of the first year (FY1), doctors will gain full registration with the GMC and will be able to apply for further study and training in a specialised area, such as psychiatry – for psychiatry, this first stage is known as Core Psychiatry Training (CT).
Specialty Training in Psychiatry
The UK Specialty Training programme in Psychiatry is 6 years long, and whilst doctors may pass through training quicker depending on how quickly they achieve their competencies, this is rarely the case and psychiatrists will usually take the indicated time, or slightly longer to complete the Specialty Training programme.
Successful applicants entering year one of core psychiatry training (CT1), will follow the Royal College of Psychiatrists’ 2017 Specialist Training in Psychiatry Curriculum.
The Psychiatry training programme
The psychiatry specialty training scheme operates both as a run-through and uncoupled programme, though it is more often un-coupled.
Depending on where your application is successful, you may complete your period of core training, as well as the Royal College exams before making a further application for the next stage of training (requiring two applications). Alternatively, you may be able to apply for run-through training, which guarantees you complete both Core and Higher training in one region, as you are recruited for the full duration of Specialty Training.
Foundation Training (FY1 – FY2)
The foundation programme usually involves six different rotations or placements in medical or surgical specialties. These rotations enable trainees to practise and gain competence in basic clinical skills.
Selection
Here, trainees will either choose whether to enter GP (General Practitioner) training, internal medicine training (IMT) or core training in psychiatry (CT).
Core Psychiatry Training (CT1 – CT3)
This part of training takes place from year 1 to 3, where trainees will work and train in several different sub-specialties within psychiatry. They will gain a broad understanding of psychiatry by rotating between 6-month posts in the following sub-specialties:
General and Community Psychiatry - including Assertive Outreach, Crisis Home Treatment, Outreach for Homeless People, Early Intervention for Psychosis, Rehabilitation and Liaison Psychiatry.
Old Age Psychiatry - including Memory Clinics, Community Teams, Domiciliary Clinics, Young Onset Dementia, Day Hospital and Liaison Psychiatry.
Child and Adolescent Psychiatry - including Specialist Adolescent and Academic Psychiatry.
Substance Misuse
Learning Disability Psychiatry - including Specialist Asperger Services.
Forensic Psychiatry - including all levels of security.
By the end of CT3, trainees will need to have completed the MRCPsych exams.
Please note, trainees must pass the MRCPsych Paper A, Paper B and CASC exams in order to progress to higher psychiatry training.
For more information of the Royal College of Psychiatrists examination suite, take a look at our IMG Resources library here.
There are two opportunities per year to apply to core psychiatry training. Information about how to apply, including the person specifications, is available via the North West Deanery, who manage the recruitment process.
Selection
Here, trainees who are not currently training in a run-through programme will make applications to a deanery for higher psychiatry training in their chosen specialty. Selection is open by national competition.
Higher Psychiatry Training (ST4 – ST6)
This training takes place from years 4 – 6, where trainees will complete 3 years of yearly rotations in their chosen speciality, building on their core training and develop increasing levels of competence in clinical psychiatry.
There will also be opportunities to work in other sub-specialties including: addictions, eating disorders, neuro-psychiatry, perinatal and social & rehabilitation psychiatry.
Trainees will usually be allocated a certain number of PAs (programmed activities) weekly for special interest or research purposes. As well as sub-specialty opportunities, these can also be used towards educational opportunities such as local training days/conferences in relevant domains, from clinical leadership to humanities.
Completion of the Psychiatry Specialty Training Programme
Upon completion of the training programme, the choice is made as to whether the trainee will be awarded a Certificate of Completion of Training (CCT) in General Adult Psychiatry of one of its sub-specialisms. This will be based on criteria set out in the curriculum by the Royal College. You can find the 2021 curriculum here.
At this point, the psychiatrists are entered onto the specialist register and can now take permanent consultant posts in the NHS.
Specialist Registration for overseas doctors
Doctors who completed part or all of their psychiatry training outside of the UK are eligible for specialist registration through the CESR or CESR-CP pathways. To learn more about specialist registration for overseas doctors, read our blog here.
Joining the Psychiatry Specialty Training Programme as an IMG
It is possible for overseas doctors to join the Specialty Training programme in Psychiatry in the UK, however it is very competitive.
IMGs interested in UK specialty training must have:
Full GMC registration
Completion of a minimum 12-month (FY1 equivalent) internship
English language test
PLAB
AND
12 months post-internship experience by the time you start begin ST1
Although UK trainees are not given priority for specialty training places, it can be very difficult to join the Psychiatry Specialty Training programme without NHS experience.
So here you have it, a broad overview of the NHS Psychiatry Specialty Training pathway for UK trainees. This training scheme is the core of psychiatry training in the UK, and for IMGs looking to join the training programme, understanding of the pathway allows you to better align your overseas training with the relevant stage you wound enter into Specialty Training in the UK.
Getting started
If you have any further questions about the UK training pathway or your route to the UK as an overseas psychiatrist, or would like guidance in finding NHS posts which offer CESR support, please get in touch with us here.
For access to a community of like-minded MRCPsych aspirants and dedicated psychiatry recruiters, join the IMG Psychiatrists Facebook group.
To receive the latest news and updates on all things psychiatry, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.
UK Training Pathway for Clinical Oncologists
The NHS specialty training programme for clinical oncologists is recognised around the world. The quality and depth of oncology training and career development in the UK is recognised as a gold standard across the globe, making it a major attraction for many IMGs when considering a career in the UK.
The NHS training programme for oncology trainees is regularly reviewed and updated, in keeping with advances and progression in the landscape of oncology around the world and throughout the profession.
In this article, we will explore the training pathway for clinical oncologists in the UK, covering the following topics:
What is the NHS Training Pathway?
How do you enter the training pathway?
What does the specialty training programme look like for clinical oncology?
What happens after completing the clinical oncology training programme?
Can I enter specialty training in the UK as an IMG?
Skip ahead to the relevant section if you know what you’re looking for.
The NHS Training Pathway for Clinical Oncologists
The NHS training pathway refers to the complete programme undertaken by UK trainees, from medical school to the completion of specialist training and being awarded a CCT.
It is a good idea for overseas trainees to familiarise themselves with this as it helps to provide an understanding of at what stage they can most likely enter the system, either in a training or non-training post.
Entering the NHS Training Pathway
After graduating from medical school, doctors receive provisional GMC registration, allowing them to enter the Foundation programme (a two-year work-based training programme).
Upon completion of the first year of this programme (FY1), doctors will gain full GMC registration with license to practice and will be able to apply for further study and training in a specialised area i.e. medicine. This is known as Internal Medicine Training (IMT), formerly known as Core Training (CT).
Specialty Training in Clinical Oncology
The Specialty Training programme in Clinical Oncology runs over a 6-year period, and doctors will usually take the indicated time, or slightly longer to complete the Specialty Training programme.
Successful applicants entering into year one of specialty training (ST1), will follow the Royal College of Radiologists’ 2021 Clinical Oncology Specialty Training Curriculum, which sets the expected syllabus as well as required assessments and workload case numbers.
Clinical oncology training as an uncoupled programme
Clinical oncology specialty training begins at ST3, so after foundation training, there are two options open to trainees before they can start specialist clinical oncology training:
Internal Medical Training (IMT)
Acute Care Common Stem (ACCS)
For IMT, this is a two-year training period and the ACCS training programme lasts 3 years.
Both pathways are followed by an open competition to enter a higher specialty training post. It is important to note that the application following core training is competitive and does not guarantee a specialty training post.
Clinical oncology higher specialty training is indicatively a five-year clinical training programme (including Oncology Common Stem), leading to single accreditation in clinical oncology.
There are a few critical progression points during higher specialty training in clinical oncology, and trainees will also be subject to an annual review of progress via the ARCP process. They will have to complete all the curriculum requirements including passing the MRCP and FRCR (Oncology) exams prior to obtaining CCT.
Foundation Training (FY1 – FY2)
The foundation programme usually involves six different rotations or placements in medical or surgical specialties. These rotations enable trainees to practise and gain competence in basic clinical skills and forms the bridge between medical school and speciality training.
This first year of Foundation Training (or FY1) is referred to as an internship. For IMGs applying for GMC registration, it is essential you can meet the requirements for an internship.
Selection
Here, trainees will either choose to either Internal Medicine Training (IMT), Acute Care Common Stem training (ACCS), or training to become a general practitioner (GP Training).
Specialty Training (ST1 – ST7)
Internal Medicine Stage 1 Training (ST1 – ST2)
Year one trainees begin at ST1 of the Internal Medicine Training Programme. In this first stage, trainees develop a solid foundation of professional and generic clinical capabilities, preparing them for participation in acute medicine at a senior level and to manage patients with acute and chronic medical problems in outpatient and inpatient settings. The curriculum for IMT Stage 1 Training can be found here.
The two-year training period culminates in trainees sitting the MRCP (UK) exams. For more information on the Royal College of Physicians examination suite, take a look at our IMG Resources library here.
Please note, trainees must have gained full MRCP prior to beginning Specialty Training in Oncology.
Selection
Here, trainees will either choose to continue with Internal Medicine Training for a further year, to continue with training in a specialty that supports acute hospital care, or to provide primarily out-patient based services in e.g. oncology.
Clinical oncology recruitment into ST3 posts usually occurs after 2 years of Internal Medicine Stage 1 training. However, trainees who complete the full three-year IMT programme are also eligible and there is no preferential selection for trainees who have completed either two or three years of training.
Oncology Common Stem (ST3)
The Oncology Common Stem (OCS) has a duration of one year and usually takes place in year 3 of specialty training (ST3). Here, the focus is on a trainee’s development of generic capabilities-in-practice (CiPs) expected of all doctors, as well as the common CiPs relating to the key areas of overlap between medical and clinical oncology.
Clinical Oncology and Medical Oncology are the two main medical specialities that manage patients with non-haematological malignancy. They often work in partnership with each other, and both offer systemic therapy to patients, but only clinical oncologists administer radiotherapy and there are other differences in work-pattern, approach and focus.
During OCS training, trainees will gain knowledge of radiotherapy planning and delivery. This will enable them to coordinate the care of cancer patients with the wider multidisciplinary team (MDT), managing patients throughout a treatment pathway.
The new curricular structure of the OCS means that trainees who successfully complete the training year will have gained the necessary competencies to progress to ST4 in either clinical or medical oncology.
For oncologists wishing to pursue clinical oncology, the first exam in the Fellowship of the Royal College of Radiologists assessment series, First FRCR (Oncology) (Part 1/ CO1), must be passed by the end of ST4.
Candidates do not need to have held a clinical oncology training post to attempt the exam however, so candidates are eligible to sit the exam during ST3.
Click here to learn more about the full FRCR (Oncology) examination suite.
Clinical Oncology Specialty Training & Maintenance of Common Capabilities (ST4 – ST7)
Once trainees have completed the OCS, they will then move onto a subsequent higher specialty-specific programme of their choice I.e. clinical oncology. This programme lasts for four years and takes place from ST4 to ST7, the focus here being to acquire clinical oncology specific CiPs, culminating in trainees’ achievement of Fellowship of the Royal College of Radiologists (FRCR Oncology).
The higher specialty-specific programme for clinical oncologists is administered by the Royal College of Radiologists, so the Medical Oncology SCE is not a requirement for clinical oncologists.
Trainees will then sit the Final FRCR (Oncology) Part 2A and 2B exams (CO2A and CO2B), usually from ST6 to ST7. This is to assess their knowledge and skills related to the investigation of malignant disease and the care and management of patients with cancer.
Completion of the Clinical Oncology Specialty Training Programme
Upon completion of the clinical oncology training programme, the choice is made as to whether the trainee will be awarded a Certificate of Completion of Training (CCT) in Clinical Oncology. This will be based on high-level learning outcomes – capabilities in practice (CiPs) set out in the curriculum by the Royal College. You can find the 2021 curriculum here.
At this point, clinical oncologists are recommended to the GMC for the award of CCT and entry onto the specialist register for clinical oncology and can now take permanent consultant posts in the NHS.
Specialist Registration for overseas doctors
Doctors who completed part or all of their clinical or radiation oncology training outside of the UK are eligible for specialist registration through the CESR or CESR-CP pathways. To learn more about specialist registration for overseas doctors, read our blog here.
Joining the Clinical Oncology Specialty Training Programme as an IMG
It is possible for overseas doctors to join the Specialty Training programme in Clinical Oncology in the UK, however it is very competitive.
IMGs interested in UK specialty training must have:
Full GMC registration
Completion of a minimum 12-month (FY1 equivalent) internship
English language test
PLAB or a recognised European Medical Degree
AND
12 months post-internship experience by the time you start begin ST1
Please note, whilst UK trainees are not given priority for specialty training spaces, it can be extremely difficult to join the Specialty Training programme if you do not have previous NHS experience.
So there you have it, the NHS Specialty Training pathway for clinical oncology trainees. The training programme forms the basis of clinical oncology training in the UK, and for overseas clinical or radiation oncologists interested in joining the training programme, good knowledge of the pathway allows you to better understand the alignment of your overseas training with the relevant stage of Specialty Training for clinical oncology in the UK.
Join the IMG Oncologists Facebook group for access to a community of like-minded oncologists and dedicated oncology recruiters.
In this group you will find tailored resources for oncology IMGs, including access to our FRCR (Oncology) crash courses, completely free to all doctors.
You can access our IMG Oncologists community here.
For regular news and updates on the Royal College and all things oncology, follow IMG Connect on social media using the links below:

Medical Training Initiative (MTI) – a comprehensive guide for doctors
Here we take a closer look at the Medical Training Initiative (MTI), a placement scheme for more junior overseas doctors to come to the UK to receive training and development within the NHS.
To be eligible for an MTI post, certain criteria must be met. These are summarised below along with a broad look the following:
What is the Medical Training Initiative?
What training will I receive through the MTI?
Am I eligible for an MTI post?
What does the application process for the MTI involve?
What are the advantages and disadvantages of the MTI?
Do I need a visa for the MTI?
How can I use the MTI for GMC registration?
How much will I be paid throughout the MTI?
What is the full process for MTI?
I’ve completed the MTI, what’s next?
Skip ahead to the relevant section if you know what you’re looking for.
The Medical Training Initiative
The Medical Training Initiative, or MTI, is a training programme that provides junior doctors from all over the world the opportunity to gain clinical training and development in the UK for a maximum of 24 months.
The MTI as a training scheme is mutually beneficial for both junior doctors and the NHS, in that doctors from several countries and specialisms around the world can work and train in the UK, gaining knowledge and experience which they can take back to their home country, while giving NHS Trusts a high-quality, longer-term alternative for unfilled training vacancies and rota gaps.
Training
The training provided through the MTI scheme will vary between programmes; however, it will typically follow the CCT curriculum (Certificate of Completion of Training). The level of training will be highly dependent on the doctor’s interests, competence and the training available within the placement hospital.
At the beginning of each placement, doctors are allocated an Educational Supervisor who will help to set the doctor’s specific training objectives to meet over the 24 months of the placement.
Eligibility
The MTI has been designed specifically with junior doctors in mind, therefore sponsorship will not be offered to consultants, specialty doctors or for locum-appointed service posts (LAS).
The criteria also differ among MTI programmes, so eligibility criteria should be checked directly with the Royal College before applying. However, the general elements of eligibility include the following:
Country requirements - priority is given to doctors from countries classified as low income or lower middle income by the World Bank. Doctors from outside of these countries may also apply, but there may be a long wait time and no guarantee of acceptance.
Evidence of skills and knowledge – the requirements for evidence of skills and knowledge vary based on the MTI programme, but the potential requirements for evidence of skills and knowledge include:
PLAB exams
Part 1 of relevant Royal College exam e.g. MRCP
Specialist qualifications from your home country
Evidence of English language skills - almost all MTI programs accept what test is approved by the GMC, meaning either of the IELTS or OET can be used for MTI.
Sufficient clinical experience - most MTI programmes will require a minimum of three years' experience, including one year of internship and one year in the relevant specialty.
Active medical practice - candidates must have been actively practicing clinically for at least three out of the last five years including the past 12 months before the application as well as throughout the application process.
The Application Process
There are two ways to join the MTI programme:
Apply for an MTI-match programme – certain specialisms have programmes which match doctors to a job. For these, you apply for the relevant programme, providing the necessary documentation. If your application is successful, you will be allocated a suitable job, which can take up to 12 months.
Find an NHS job before applying for the MTI – in cases where specialties do not have an established match programme, candidates are required to apply directly for an NHS post. Once the candidate has been accepted for the role, they can then apply for the MTI scheme through the relevant Royal College. If you would like to know more about finding NHS posts for the MTI scheme, you can get in touch with us here.
Specialties may use either, or a combination of these two methods, so we suggest visiting the Royal College and searching for their information on the MTI scheme.
The availability of MTI posts will vary between each Royal College, as certain specialties are more consultant-led, meaning there are fewer training posts for junior doctors. Once again, we suggest finding out more from the relevant Royal College.
Advantages and Disadvantages of the MTI Scheme
Advantages
Training – MTI doctors will receive training and development support in their clinical, communication and leadership skills, as well as supervision by a consultant. You will also have the opportunity to create a training plan with the support of an Educational Supervisor.
Reduced cost – for posts that accept specialist qualifications from the applicant’s home country, the associated costs are lower as you will not have to pay for the PLAB or Royal College exams which can be costly, especially where retakes are needed
Alternative to PLAB and the Royal College – As some posts accept a candidate’s specialist qualifications from overseas, this allows you to bypass the Royal College and PLAB exams (N.B. if you have passed both parts of PLAB or ever failed either of the exams, you are not eligible for MTI)
Diploma of UK Medical Practice - If you complete an MTI post that is at least 12 months long, with the Royal College of Physicians (RCP) or the Royal College of Paediatrics and Child Health (RCPCH), you can apply for the DipUKMP, a professional diploma which can be used as part of the portfolio of evidence required for specialist registration (CESR or CESR-CP).
Disadvantages
Not all posts are paid - Some MTI posts require you to secure funding for your training, for example through scholarships or funding from an organisation in your home country, such as a government agency or university (N.B. personal funds cannot be used).
Junior posts – More senior doctors wanting to take this route to the UK will receive a lower salary and more junior role than if taking the postgraduate route.
British citizenship or ILR - For doctors who wish to make a permanent move to the UK, the 12-24 months spent in the UK on the MTI scheme will not count towards the 5-year requirement for British citizenship or indefinite leave to remain (ILR).
Return to home country – at the end of the 24-month period, MTI doctors are legally required to leave the UK and return to their home country.
MTI Posts Offer Tier 5 Visas
MTI candidates require a Tier 5 visa to travel to the UK. Applications for the visa can only be made after receiving the Certificate of Sponsorship.
Applications for Tier 5 visas must be made from your home country (or the country you work in), but never from the UK.
The visa must only be used for travel to the UK at the beginning of the placement and will activate after your arrival, lasting for exactly two years from your arrival date.
Please note that Tier 5 visas cannot be extended.
GMC Registration
All doctors practicing in the UK MUST be registered with the GMC. For MTI candidates, registration is typically supported by the Royal College, but some NHS Trusts also have the right to register MTI doctors.
English Language Testing
As always with GMC registration, candidates will also need to provide evidence of English language skills. This can be done by passing either the IELTS (International English Language Testing System) or the OET (OET – Occupational English Test). Detailed guides to these tests can be found below:
IELTS – a guide for overseas doctors
OET – a guide for overseas doctors
Pay Received for MTI Posts
MTI posts are either paid, or candidates are required to secure funding for their placement as detailed above.
Where the placements are paid, the salary received by the MTI doctor corresponds to trainees at a similar level in the UK. All trainees can expect to commence their MTI training at an equivalent salary to ST3 level.
Some hospitals may take prior international experience into account while others do not. This is at the discretion of the hospital and not the Royal College. Hospitals can also decide whether to employ MTI doctors under the 2002 or 2016 junior doctor contract, which have slightly different pay scales.
Therefore, it's best to verify as early as possible where your placement will be paid, whether your prior experience will be taken into account, and under what pay scale you will be paid.
Steps through MTI
We’ve detailed the general processes involved in MTI below, from a candidate’s initial application for a post, to their final interview with the Royal College after gaining GMC registration:
I’ve completed the MTI, what’s next?
Ordinarily, on completion of the MTI scheme, doctors return to their home country with the training and experience they gained from working in the NHS.
Some doctors may want to remain in the UK after completing the MTI for a number of reasons. This can be done if the doctor finds another NHS post, in which case, they may be able to switch from the Tier 5 visa to the Tier 2 Health and Care Worker visa. For more information on the Health and Care Worker Visa, please see here.
If you want to find another NHS post after completing the MTI, applying for your first NHS job follows the same process as any other doctor. You will need to consider what job it is you would like to obtain and what location in the UK you would prefer to relocate to. For guidance on jobs in your specialty in the UK, please see our IMG Resources library.
Once you are ready to start the application process you can get in touch with us – IMG Connect can offer you expert advice and representation throughout the recruitment and relocation process.
For regular news and updates on the Royal Colleges, GMC registration and working in the NHS, follow us on social media and join the conversation below:

Training, Development & Career Progression in Emergency Medicine
One of the main reasons that overseas doctors want to work in the Emergency Medicine departments across the UK, is the excellent opportunity for access to training such as the Specialist Training Programme, career progression, including CESR, and sub-specialty development.
This short article provides useful information on the training and development available, how to access the training, the best route to becoming a consultant in the UK with entry to the specialist register, no matter what stage of your training.
Emergency Medicine Training, leading to CCT
We start with an overview of the Emergency Medicine Training in the NHS. Trainees may enter the emergency medicine training programme via:
The EM (Emergency Medicine) core training programme at ST1. This is a three-year core training programme (starting from ST1 and ending at ST3).
For the first two years, trainees will spend 6 months in EM, Intensive Care Medicine, Anaesthetics and Acute Medicine. This is followed by a further year in trauma and paediatric EM.
The start of specialty training (ST4-6) subject to having achieved the necessary competences required for completion of ST3.
Once ST6 is completed, then a doctor will be added to the specialist register for medicine and hold the title of CCT. This means that they can apply for and practice at a consultant level in the NHS.
CESR
For senior Emergency Medicine doctors (experienced specialty doctors, consultants and heads of departments) there is also the option of CESR. You can apply directly for CESR from overseas, or secure a post in the NHS with CESR support and complete your application in the UK. This is a good option for those wanting to take up their first role in the NHS as a specialty doctor (leading to consultant) or as a locum consultant.
Applying from abroad can be lengthy, and it is certainly not the quickest route towards specialist registration. Most IMGs prefer to secure a post with CESR support, so speak to your IMG Consultant to learn more about the best route to the UK for senior doctors seeking consultant jobs in Emergency Medicine.
Most senior Emergency Medicine job vacancies advertised will offer support with CESR, access to training and career progression, and senior managers will encourage you to develop your own professional interests.
Emergency medicine departments in the NHS are particularly supportive of doctors seeking to develop both personally and professionally. To find out what jobs are on offer take a look here.
If you think that a Specialty Doctor post with CESR support is suited to you, or if you are a consultant or head of department, then you can find out more information here.
For further advice on how to secure the right job for you in the NHS, take a look at our the following article.
IMG Jobs
Search and find live emergency medicine NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor jobs, doctor salary & relocation for emergency medicine specialists
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to see what Emergency Medicine job opportunities there are for you, including access to CESR support, Core and Specialty training.
For the latest news and updates on all things emergency medicine, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.