Search IMG Library
YOUR SPECIALISM- See all
- Gastroenterology
- Microbiology
- Urology
- Rheumatology
- Stroke Medicine
- Ophthalmology
- Oncology
- Neurology
- Histopathology
- Haematology
- ENT Surgery
- Acute Medicine
- Anaesthetics
- Respiratory
- Dermatology
- Geriatrics
- Radiology
- Surgery
- Paediatrics
- Psychiatry
- Emergency Medicine
- Critical Care & ICU
- General Medicine
276 blogs found
CESR Applications for Medical Oncologists
In this article, we’ll be taking a closer look at the specific guidance on NHS applications for entry onto the Specialist Register through the Certificate of Eligibility for Specialist Registration (CESR) for medical oncologists.
We’ll cover the eligibility criteria, application process, and most importantly the required evidence, along with some other topics, summarised in the headings below:
What is CESR and who is it for?
Do overseas oncologists need MRCP for CESR?
What is the CESR equivalence process?
What evidence is required for a CESR in medical oncology?
Where will I find this evidence?
How do I submit a CESR application?
How long does it take to complete?
How much does CESR cost?
How long does it take to receive a decision?
#IMG Tips
How do I get started?
Skip ahead to the relevant section if you know what you’re looking for.
An Introduction to CESR
CESR, or the Certificate of Eligibility for Specialist Registration, is the route to specialist registration for doctors who have not completed a GMC-approved training programme, but can demonstrate that their specialist training, qualifications and experience are equivalent to the requirements for the award of the CCT in the UK.
CESR holders can be appointed to substantive (or permanent) consultant positions in the NHS. As a medical oncologist, attaining specialist registration will mean you are qualified to practice independently as a consultant in the NHS.
Oncologists must prove to the GMC that their specialist training or specialist qualifications, when considered together, are equivalent to a CCT in the specialty in question.
In order to be eligible for CESR, doctors should have undertaken a minimum of 6 months training or obtained a specialist qualification and acquired specialist medical experience or knowledge as a medical oncologist within a non-training post.
Overseas doctors do not require CESR before moving to the UK to work in the NHS. Often, experienced oncologists will secure a post in the UK, and work towards CESR whilst in post.
MRCP for Specialist Registration
Whilst it is always beneficial to complete MRCP (UK), particularly for doctors who have trained outside the UK or the EEA, overseas doctors looking to join the Specialist Register do not need to have completed the Royal College postgraduate exams.
The standard test of knowledge in the Medical Oncology curriculum is the MRCP (UK) exams, so passing these exams confirms the attainment of the competencies of the core curriculum.
MRCP (UK) is only a requirement for doctors looking to attain Specialist Registration via the CCT or CESR-CP route.
The structure of medical oncology training in the UK is an indicative two years in Core Medical Training or Acute Care Common Stem (ACCS), followed by an indicative four years of training in Medical Oncology. Therefore, applicants need to demonstrate the appropriate level of acute medicine expertise as well as competencies in medical oncology.
You can read more about the evidence required in the specialty specific guidance here.
CESR Equivalence Process
Equivalence refers to the process of assessing an overseas applicant’s training and experience against the current medical oncology training programme requirements, in order to be awarded CESR.
The equivalence process involves submitting a written body of evidence to the GMC, consisting of:
training and/or competence; AND
skills and knowledge
The Royal College of Physicians will assess each application against the relevant curriculum before providing a recommendation to the GMC, who will then make a decision.
Please note that Equivalence procedures are the responsibility of the GMC. Applications are made through their Certification Department and initial enquiries should be directed there.
Evidence Requirements for CESR in Medical Oncology
Skills & Experience: The evidence provided for a CESR application in oncology must cover the knowledge, skills and qualifications to demonstrate the required competencies in all areas of the Medical Oncology curriculum. If evidence is missing from any area of the curriculum, the application will fail.
Primary Evidence: To demonstrate that you can do what is required by the curriculum, you need to submit primary evidence of your clinical practice which shows how you work on a day-to-day basis: letters, reports, assessments etc. References, retrospective case summaries, and reflective notes can all be used in a CESR application, but by themselves they are not sufficient.
Audit & Governance: You are required to submit evidence of your active leadership in audit, including evidence that you have completed at least one audit cycle
Currency of Evidence: Your evaluators will be looking for evidence of current competency, generally defined as within the last five years. If you have completed training before this point, it is crucial that you provide evidence of maintaining competency across the whole area of the curriculum.
The GMC asks that only evidence that is strictly relevant is sent as it will help them to process the application quicker. The guidance on compiling your evidence will help you to decide what is relevant and what is not – you can find this on the GMC website here.
As a general guide, the GMC usually expects to see about 800 - 1000 pages of evidence, divided into four different domains, reflecting those of Good Medical Practice. The GMC recommends that you apportion the evidence provided as shown below:
Domain 1 – Knowledge, skills and performance
Domain 2 – Safety and quality
Domain 3 – Communication, partnership and teamwork
Domain 4 – Maintaining trust
Please note, you cannot compensate for evidence lacking in one area by providing more evidence in another area.
The full list of evidence required for each domain can be found on the GMC website here.
Gathering Evidence for a CESR Application
Domain 1 – Knowledge, skills and performance
Qualifications
Primary Medical Qualification (PMQ)
Specialist medical qualification(s)
Curriculum or syllabus (if undertaken outside the UK)
Specialist registration outside the UK
Honours and prizes
Other relevant qualifications
Assessments and appraisals
Appraisals and assessments
RITAs, ARCPs and training assessments
360˚ and multi-source feedback
Awards and discretionary points letters
Personal development plans (PDP)
Logbooks, records of daily clinical practice and portfolios
Logbooks
Consolidation, cumulative data sheets, summary lists and annual caseload statistics
Medical reports
Case histories
Referral letters discussing patient handling
Patient lists
Departmental (or trust) workload statistics and annual caseload statistics
Rotas, timetables and job plans
Courses relevant to curriculum
Portfolios (electronic or revalidation)
Details of posts and duties (including both training and experience posts)
Employment letters and contracts of employment
Job descriptions
Job plans
Research, publications and presentations
Research papers, grants, patent designs
Publications within specialty field
Presentations, poster presentations
CPD and CME
CPD record certificates, certificates of attendance, workshops and at local, national and international meetings or conferences
CPD registration points from UK Medical Royal College (or equivalent body overseas)
Membership of professional bodies and organisations
Teaching timetables
Lectures
Feedback or evaluation forms from those taught
Letters from colleagues
Attendance at teaching or appraisal courses
Participation in assessment or appraisal and appointments processes
Domain 2 – Safety and quality
Participation in audit, service improvement
Audits undertaken by applicant
Reflective diaries
Service improvement and clinical governance meetings
Safety
Health and safety
Domains 3 - Communication, partnership and teamwork
Communication
Colleagues
Patients
Partnership and teamwork
Working in multidisciplinary teams
Management and leadership experience
Chairing meetings and leading projects
Domain 4 – Maintaining trust
Acting with honesty and integrity
Honest and integrity
Equality and human rights (including disability, human rights, race, religion and ethnicity awareness and equal opportunities)
Data protection
Relationships with patients
Testimonials and letters from colleagues
Thank you letters, cards from colleagues and patients
Complaints and responses to complaints
For more guidance on the different types of evidence, see the specialty specific guidance from the GMC for medical oncology.
Validating Evidence
Original documents which are on headed paper with a hospital stamp and original signatures do not need additional validation.
All photocopied evidence should contain a hospital stamp on every page of each document, the validator’s name (printed and in full), job title (printed and in full) and original signature.
Application Submission
All CESR applications are submitted online via GMC Online and if you have not already created an account, you can find a guide on how to do so here.
Electronic evidence is required for each of the different evidence sections of the CESR application. Once started, the online application remains open for 12 months, meaning that it can be used as a portfolio to gather evidence against each of the different sections.
Your electronic evidence can be in any of the following formats:
.doc
.pdf
.ppt
.xls
Formats outside of these are unlikely to be accepted.
The Online Application
You will be required to complete the following sections once you begin your application:
Specialty details
Qualification details and professional experience
Details of your referees
Registration and licensing history
Evidence summary
Details of your verifiers
Final declaration and payment
Additional Evidence
Once an Adviser on the Specialist Applications Team has reviewed your initial evidence, they will provide you with information on:
What evidence they’ve accepted
What evidence they’re unable to accept (including the reasons for this)
Advice and guidance on how your application could be strengthened
You’ll have up to 60 days to provide additional documentary evidence in support of your application (30 days if you’ve submitted a Review application).
For further information about the online application process, see the GMC’s User Guide.
How long does it take to complete?
As there is a substantial amount of evidence to gather for a CESR application, the process of preparing all the necessary documentation and applying for CESR can take even longer than this, and a typical candidate will usually set out to complete this within 1 – 3 years.
It is worth noting that more senior oncologists, such as consultants, are more likely to have achieved all the competences outlined in the curriculum.
The indicative period of training for a CCT in medical oncology is six years, so it is highly unlikely that you would achieve the competencies required for a CCT in a shorter period of time. Therefore, CESR is not suitable for more junior oncologists.
Cost of CESR Applications
All oncologists applying for Specialist Registration must pay a fee. For CESR, this fee is £1,727.
For CESR-CP and CCT, the cost is £452.
How long does it take to receive a decision?
The GMC estimate that it can take between six and eight months to receive a decision, from the date you submit your CESR application.
#IMG Tips
Research/think about the types of evidence you will need and begin to gather your evidence well in advance of making your application.
Gather evidence prospectively – this is much easier than retrospectively trying to pull together the evidence under additional pressures.
Make sure that your evidence is of the highest possible quality and is current – you will be assessed against the most recent curriculum.
Ensure that the evidence you collect demonstrates your competence across the whole of the Medical Oncology curriculum, not just your sub-specialty.
Remember to refer to the most up-to-date Medical Oncology CCT Curriculum and Specialty Specific Guidance for the evidence requirements in your specialty.
Create a CESR ‘to-do list’ with sections under the GMC’s 4 domain headings – organise your evidence directly into these sections to manage your progress.
Do not submit original documents – all your copies, other than qualifications you’re getting authenticated must be accompanied by a proformas signed by the person who is attesting to the validity and accuracy of your evidence (your verifier).
Ask an IMG Connect recruitment specialist about NHS oncology posts with CESR support. These are not always advertised by a Trust, but we can help you find a role which aligns well with your career goals in the NHS.
Join the online community - join the IMG Oncologists Facebook group for access to a community of like-minded MRCP aspirants and dedicated oncology recruiters.
In this group you will find tailored resources for oncology IMGs, including access to our MRCP crash courses, completely free to all doctors.
You can access our IMG Oncologists community here.
Sources
https://www.jrcptb.org.uk/certificate-eligibility-specialist-registration
https://www.gmc-uk.org/registration-and-licensing/join-the-register/registration-applications/specialist-application-guides/specialist-registration-cesr-or-cegpr
https://www.gmc-uk.org/-/media/documents/sat---ssg---medical-oncology---dc2310_pdf-48455474.pdf
Getting started
Attaining Specialist Registration through the CESR pathway can be a long but very rewarding process. Look at our introduction to CESR for medical oncologists for a full overview.
If you have any further questions about Specialist Registration, your route to the UK, or would like guidance in finding NHS posts which offer CESR support, please get in touch with us here.
Follow us on social media through the links below for regular news and updates on the Royal Colleges, relocating to the UK and working in the NHS:

Medical Training Initiative (MTI) for Medicine Doctors
Here we take a closer look at the Medical Training Initiative (MTI) for international doctors practicing medicine and its sub-specialties.
Whilst the MTI describes a UK-wide placement scheme for junior overseas doctors, the processes involved vary between specialties.
This blog focuses on the MTI scheme as administered by the RCP, and the particular of this are summarised below along with a broad look the following:
What is the Medical Training Initiative?
What is the RCP and what support does it provide throughout my training?
Am I eligible for an MTI post?
Are there any additional requirements for the RCP?
How can I use the MTI for GMC registration?
What does the application process for the MTI through the RCP involve?
How am I supported in obtaining a visa?
I’m coming to the end of the MTI, what’s next?
Skip ahead to the relevant section if you know what you’re looking for.
The Medical Training Initiative
The Medical Training Initiative, or MTI, is a training programme that provides junior doctors from all over the world the opportunity to gain clinical training and development in the UK for a maximum of 24 months.
The MTI as a training scheme is mutually beneficial for both junior doctors and the NHS, in that doctors from several countries and specialisms around the world can work and train in the UK, gaining knowledge and experience which they can take back to their home country, while giving NHS Trusts a high-quality, longer-term alternative for unfilled training vacancies and rota gaps.
Royal College of Physicians (RCP)
The Royal College of Physicians is the professional body that regulates medicine specialties in the UK, and Membership of the Royal College of Physicians (MRCP) is the full qualification attainable by examination.
Take a look at IMG Resources library for complete guides on MRCP to learn more.
There are several ways you will be supported by the RCP as listed below:
Induction – all MTI candidates are expected to attend an induction at the RCP. The induction is held on a quarterly basis
Free ePortfolio access – this is an electronic portfolio to log all your assessments and training whilst in the UK
Free RCP associate membership – this is for the first year and discounted rate for the second year and comes with a number of benefits
Annual symposium – this is a clinical conference for all RCP MTIs held once a year
Diploma in UK Medical Practice – participants are required to carefully document their training using the ePortfolio system, complete a range of continuing medical education sessions, and submit a written reflection piece at the end of their placement
RCP certificate - at the end of training there is an RCP certificate available to all candidates
Support for any issues that you might encounter relating to your training
Eligibility
The MTI has been designed specifically with junior doctors in mind, therefore sponsorship will not be offered to consultants, specialty doctors or for locum-appointed service posts (LAS).
The eligibility criteria differ among MTI programmes, but for the RCP, eligibility includes the following:
Country Requirements - Priority is given to doctors from countries classified as low income or lower middle income by the World Bank and priority countries as described by the Department for International Development. Doctors from outside these countries may also apply, but there may be a long wait time and no guarantee of acceptance.
Primary Medical Qualification: You must hold a recognised PMQ by the GMC and verified by Educational Commission for Foreign Medical Graduates (ECFMG)
Have a Postgraduate Medical Qualification: This can be MRCP Part 1, MD or other higher degree in medicine or a medical subspecialty
Skills & Competencies: You must possess the skills, competencies and understanding of medicine at least equivalent to a UK graduate at the end of their core medical training.
Clinical Experience: You must have 3 years post-qualification experience, including 1 year's internship and at least 1 year in the specialty in which you intend to train while in the UK
Active Medical Practice: Candidates must have been actively practicing clinically for at least three out of the last five years including the past 12 months before the application as well as throughout the application process (the GMC does not consider clinical observerships as clinical practice).
Please note, the RCP cannot sponsor doctors who have failed the Professional and Linguistic Assessments Board (PLAB) test.
Additional Requirements
Before you can make an application for the MTI scheme through the RCP, the following criteria must be satisfied:
Verification of PMQ – your primary medical qualification must be independently verified by the ECFMG via their EPIC service.
Complete an English Language test – the test must have been completed within two years of application for GMC registration.
Find an NHS job before applying for the MTI – you are required to apply directly for an NHS post and should have already been formally offered the role before contacting the RCP. The hospitals should also be in support of your intention to seek sponsorship for the post.
Obtain funding - you should already have funding for your post from either a scholarship, official funding, or a salary. The funding should be equivalent to a UK salary for the level of work being undertaken and must last for the duration of the post. The RCP will not sponsor applicants who are self-funded.
Certificate of Good Standing - you must be able to provide a certificate of good standing (CGS) from the regulatory body in the countries where you have practised in the last 5 years. The CGS should be no older than 3 months when submitted.
GMC Registration
All doctors practicing in the UK must be registered with the GMC. For MTI candidates, registration is typically supported by the Royal College, but some NHS Trusts also have the right to register MTI doctors.
English Language Testing – candidates will also need to provide evidence of English language skills. This can be done by passing either IELTS with overall score of 7.5 and 7.0 in all categories or OET with minimum grade B in all categories. Further information on these tests can be found below:
IELTS – a guide for overseas doctors
OET – a guide for overseas doctors
Application Process
Once you fulfill all the eligibility criteria and additional requirements laid out by the RCP, you must complete the initial and professional postgraduate experience (PPE) forms and email these along with your CV to mti@rcplondon.ac.uk.
Once your CV, initial form and PPE forms have been received, the RCP will contact the supervising consultant in the UK and confirm the details of your post. You will then be sent an application pack. You should complete the application form and send it to the RCP with all of the following documents:
sponsor form (forms will be provided by the RCP) – must be completed by your consultant or head of department in your home country
two reference forms (forms will be provided by the RCP)
copy of your passport
copy of your IELTS/OET certificate or details of exemption
copies of your medical qualifications
translations of your medical qualifications if they are not in English
letter from the dean of the medical school from which you graduated
copy of certificate of good standing
letter from the UK hospital confirming your appointment
evidence of funding for the post
your statement agreeing to the level of funding which you have received from any of the sources listed
initial fee of £125
We’ve detailed the general processes involved in MTI applications through the RCP below, from a candidate securing an NHS post, to their eligibility to work in the UK after gaining GMC registration and securing a visa.
Tier 5 Visa for MTI
The MTI scheme falls under the Tier 5 government authorised exchange visa. This visa must only be used for travel to the UK at the beginning of the placement and will activate after your arrival, lasting for exactly 24 months from your arrival date.
For a Tier 5 MTI visa, the RCP needs to provide evidence regarding your post to the Academy of Medical Royal Colleges (AoMRC - the official visa sponsor) once the GMC has approved your application in order to get your Tier 5 Certificate of Sponsorship (CoS) issued.
Once your Tier 5 CoS has been issued it is your responsibility to apply for the Tier 5 visa via https://www.gov.uk/browse/visas-immigration/work-visas.
Applications for Tier 5 visas must be made in your home country (or the country you work in), but never from within the UK.
You can also apply to the AoMRC for Tier 5 dependent visas for your spouse and children, although this is not guaranteed, and you should read the UKVI requirements on this well in advance.
Please note that Tier 5 visas cannot be extended.
Sources
https://www.rcplondon.ac.uk/education-practice/advice/medical-training-initiative-resources-applicants
https://www.rcplondon.ac.uk/education-practice/advice/medical-training-initiative
https://www.rcplondon.ac.uk/file/19236/download
https://www.rcplondon.ac.uk/file/23841/download
https://www.rcplondon.ac.uk/file/4534/download?token=QyAzDCP8
What are my options after I complete the MTI?
Ordinarily, on completion of the MTI scheme, doctors return to their home country with the training and experience they gained from working in the NHS.
Some doctors may want to remain in the UK after completing the MTI for a number of reasons. This can be done if the doctor finds another NHS post, in which case, they may be able to switch from the Tier 5 visa to the Tier 2 Health and Care Worker visa.
If you want to find another NHS post after completing the MTI, you would follow the same process as any other doctor. You will need to consider what job it is you would like to obtain and what location in the UK you would prefer to relocate to.
For guidance on NHS jobs in your specialty, please see our live jobs or get in touch with us to learn more about your options in the NHS.
For regular news and updates on the Royal Colleges, GMC registration and working in the NHS, follow us on social media and join the conversation:

Benefits of SAS doctor jobs in the NHS UK
Specialty and Associate Specialist (SAS) doctors are employed in the NHS in a non-training post. An SAS doctor will have at least four years of postgraduate training, at least two of which will be in a relevant specialty.
SAS doctor jobs in the UK are paid well and the number of posts available in the UK have risen steadily over the past decade. They are an attractive way for both the NHS and IMGs to ensure doctors are secured into posts quickly.
In this article we will consider the following topics:
What is a SAS doctor?
Could I take a training post instead?
What are the benefits to a SAS role?
How do I secure a SAS doctor job in the NHS?
What is a SAS doctor?
Specialty and Associate Specialist (SAS) doctors fill NHS service roles which sit outside of Specialty Training pathways. These roles are non-training ‘service’ roles where the doctor has at least four years of postgraduate training, at least two of those being in a relevant specialty.
A variety of terms can be applied to SAS doctors, including specialty doctor, associate specialist and staff grade.
It is worth noting however that not all non-training medical roles (service posts) are SAS doctors. Service roles are available across all grades and can be commonly referred to as Trust doctors.
Could I take a training post instead?
Yes of course. Training posts in the NHS are very attractive however competition for places on these posts is highly competitive.
As such for IMGs interested in securing a place on a training post in the NHS, we advise that they should obtain a trust doctor or SAS doctor post, depending on experience, for 1 – 2 years. Following which you will be able to apply for a training post, for which you will be given priority.
Not only will this approach give you the best chance of securing excellent training and career progression opportunities in the NHS, it will also give you the chance to settle in to the UK, get to know your trust better, and help you understand the training post that will suit you the most.
SAS doctor jobs also offer very competitive rates, so whilst you are getting to know the NHS and settling into life in the UK, you can also ensure that you are financially rewarded.
What are the benefits to a SAS role?
Less competition and a route to Specialty Training
The majority of IMGs are keen to enter the specialty training pathway at some point, but competition for these positions is very high. Places are offered to UK based applicants first, then EEA applicants, finally followed by Non-EEA applicants.
As such, it can be difficult to get a training post when applying for your first NHS role.
However, competition for service roles is not nearly so competitive and following completion of one year as a Specialty doctor you can enter into the first group of applicants for specialty training.
Allowing you time to settle into the UK and NHS
Taking a service role can be a great way to allow yourself time to bed into NHS and UK culture in the first months following your move. By taking on a new culture, employer and healthcare system all at once, you may feel more comfortable taking on a SAS post, avoiding all the extra commitment and learning associated with a training role.
Quicker route to securing your first post
For overseas doctors applying for SAS posts, the process can be quicker. Less competition and a high demand for doctors will ensure that IMG Connect can secure you interviews quickly.
Financial reward
SAS posts typically offer competitive salaries, with some harder to fill locations able to offer additional incentives. Speak with your IMG Consultant for more information.
More patient focused roles and less responsibility
SAS roles are usually more focused on meeting NHS service requirements compared to trainee roles. Many doctors simply prefer a role where they can spend more time with patients and doing the job they love, without the pressured commitment to training, admin and competition that a training role brings.
Balance between work and personal life
When taking a SAS post, additional working hours and on call commitments can be optional.
You will also be given the option to increase your overall hours through weekend and shift work, which will increase your overall take home pay.
In most circumstances it is up to you how you want to approach balancing a life at home with work commitments & financial rewards.
Freedom to consider all parts of the UK
Entering a training post is not only a commitment to the programme over a number of years, but also the geographical location that the deanery covers.
By taking a service role instead, you could complete a one-two year contract, but realise the area is not for you. At this point you could take a new contract and not have to worry about giving up your hard-earned place on the training programme.
Remember, it is vital that all contracts are honoured and not only will breaking contract have a negative impact on your CV but may also damage your chances of securing your next post.
Specialist Registration is still possible
Specialist registration is still possible via the CESR route as some hospitals or Trusts will offer SAS doctors the support required with their CESR applications. However, it is likely to be a much longer process when not taking the training pathway.
In summary:
There are many reasons why a SAS post can be a great option for experienced IMGs when considering their first job in the UK, and it is clear that trust doctors are vital to the day to day running of the NHS.
Regardless of the route you wish to take, IMG Connect will support any doctor pursing either path and can offer guidance and advice throughout either process.
So how do I secure a SAS doctor job in the NHS?
You can apply for SAS doctor roles online via the NHS Jobs websites for England & Wales, Scotland or Northern Ireland.
However, working with IMG Connect can offer more jobs than are available online with the added benefit of an IMG Consultant speaking directly with services on your behalf to expedite the process and negotiate the best doctor salary for you.
For the most comprehensive selection of roles and fastest routes to the UK for Trust Doctors, register an interest or apply for trust doctor roles via our Job Search page on our website.
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss doctor job options in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.

MRCPsych - a comprehensive guide for Hong Kong psychiatrists
Many Hong Kong psychiatrists complete MRCPsych as part of their training or are at least aware of the exam. Membership of the Royal College of Psychiatrists examinations (MRCPsych) is one of the best ways for Hong Kong psychiatrists to register with the GMC and find psychiatry jobs in the NHS.
The exams can be taken by International Medical Graduates (IMGs) from any country in the world, provided certain eligibility criteria are met. Here we provide a summary of these exams from a Hong Kong perspective, along with a broader look at the topics below:
Where does MRCPsych fit in for Hong Kong Psychiatrists?
What does MRCPsych mean for Hong Kongers?
MRCPsych can lead to CESR or Specialist Registration in the UK
An overview of MRCPsych and how can Hong Kong Psychiatrists use it for GMC registration
Eligibility for Hong Kong Psychiatrists
What is the exam content and format?
Assessment Portfolio
Sponsorship Requirements
How do I apply for the exams?
How much will it cost me?
As a Hong Kong psychiatrist, where can I sit the exams?
How can I prepare for the MRCPsych examinations
IMG Tips
Passed? What next?
Skip ahead to the relevant section if you know what you’re looking for.
Where does MRCPsych fit in for Hong Kong Psychiatrists?
Postgraduate training in Hong Kong is governed by the Hong Kong College of Psychiatrists, and historically, psychiatric training in Hong Kong has aligned closely with the UK system of postgraduate education. Most psychiatrists in Hong Kong obtain membership of the Royal College of Psychiatrists (MRCPsych) as part of their post graduate training.
The structure of postgraduate training in Hong Kong also closely follows expectations for UK Trainees by covering the same 6 years of higher specialist training. In Hong Kong, the first three years of basic training incorporate the pre-MRCPsych training scheme, which gives the trainee the opportunity to take the MRCPsych examinations at a similar time in the process to the UK.
What does MRCPsych mean for Hong Kongers?
The mental health service in Hong Kong has undergone tremendous change over the last 20-30 years, developing a solid foundation in training, legislation, research and academic work. Hong Kong has fast developed a highly regarded psychiatry service and workforce. This level of training and service, coupled with membership of the Royal College of Psychiatrists (MRCPsych) means that Hong Kong Psychiatrists, including specialists and trainees, fit very well into the UK system.
Links through IMG Connect to several of the top performing trusts in the UK, has seen several Hong Kong psychiatrists flourish in the NHS, year on year.
MRCPsych can lead to CESR or Specialist Registration in the UK
With the parallels in post-graduate specialist training and qualifications like MRCPsych and FHKCPsych, and the high level of experience of Hong Kong Psychiatrists, Hong Kongers are able to enter CESR programmes successfully, gaining specialist registration in the UK reasonably quickly.
Hong Kong Psychiatrists possess the right level of skills, experience and qualifications required for a psychiatrist to apply for CESR. Upon entering the UK system, typically in a job with CESR support, HK psychiatrists can work towards completing the CESR application process with the support of their new employer, leading to being a specialist psychiatrist in the UK.
What is MRCPsych and how can Hong Kong Psychiatrists use it for GMC registration?
The MRCPsych examinations are the main component of specialty training for psychiatrists in the UK. The Royal College exams are designed to test your knowledge of basic medical sciences as well as the clinical skills required for diagnosis and management within psychiatry.
For IMGs from Hong Kong, MRCPsych is one of the two main routes to full GMC registration - you can find a range of articles covering these routes in our resource library here: Royal College or PLAB route.
For psychiatrists who wish to take more senior roles reflective of their current practice, IMG Connect advise that MRCPsych would be the best route to take, rather than PLAB.
As above, Hong Kong Psychiatrists who possess full MRCPsych can register to work in the UK. Whether 3 years into specialist training, or complete in all aspects of the postgraduate programme in Hong Kong, whether working as an Associate Consultant, Consultant or Professor, using the MRCPsych postgraduate route to GMC registration is applicable to you.
Psychiatrists in all main specialisms of psychiatry are eligible for registration and very much in demand to fill vacancies within the NHS.
A very successful route for Hong Kong Psychiatrists has been to secure a non-training post in the NHS, often appointed as a Specialty Doctor, Specialist Grade. Coupled with a developed CESR support programme, a non-training post can ensure swift progress to specialist registration in the UK. CESR will be a requirement for Hong Kong Psychiatrists to allow an appointment to a permanent consultant post.
For Hong Kong Psychiatrists who have not yet sat the examinations, in the following sections of this blog we will provide an overview of the format, dates, fees and exam centres, as well as look at how to prepare.
Eligibility for Hong Kong Psychiatrists
The MRCPsych examinations can be taken by any registered doctor in Hong Kong.
Each examination has different criteria, to complete the full MRCPsych a Hong Kong doctor must be registered with the medical council of Hong Kong, or any recognised medical board if working elsewhere overseas. They must also complete the Assessment Portfolio for Overseas Candidates demonstrating that they have complete 3 years of equivalent training.
For each part of the exam the Royal College suggest the following eligibility criteria:
MRCPsych Paper A
You are eligible for Paper A if you are a fully registered medical practitioner (in Hong Kong or elsewhere)
MRCPsych Paper B
It is a recommended to have at least 12 months experience in psychiatry before taking this examination.
Clinical Assessment of Skills and Competencies (CASC)
You have a pass in both Paper A and B; AND
You can demonstrate you have sponsorship in place. Sponsorship forms must be submitted by an appropriate medical education lead confirming that the eligibility requirements to sit the MRCPsych examinations have been met; AND
You have 24 months post internship experience in Psychiatry; AND
(Overseas candidates) Assessment portfolio
Exam content and format
The MRCPsych examinations consist of two written papers (Paper A + Paper B) and one clinical examination (CASC).
Paper A – The scientific and theoretical basis of psychiatry
This is a three-hour written paper, worth 150 marks and comprising of 150 questions made up of approximately two thirds multiple choice questions (MCQ) and one third extended matching item questions (EMI).
It covers the following sections of the syllabus:
Behavioural Science and Socio-cultural Psychiatry
Human Development
Basic Neurosciences
Clinical Psychopharmacology
Classification and Assessment in Psychiatry
Paper B - Critical review and the clinical topics in psychiatry
This is a three-hour written paper, worth 150 marks and comprising of 150 questions. The content includes one third critical review and two thirds on clinical topics.
It covers the following sections of the syllabus:
Organisation and delivery
General adult
Old age
Psychotherapy
Child & adolescent
Substance misuse
Forensic
Learning disability
Critical review
CASC - Clinical Assessment of Skills and Competencies
The CASC is based on a format similar to OSCEs. Specifically, the examination consists of two circuits which must be completed on the same day.
In total, the circuit includes 16 stations, made up of:
Five stations on history taking, including risk assessment
Five stations on examination, including physical and mental state
Six stations on patient management
Stations consist of several elements with instructions provided to all candidates, marked against the examiners construct.
These have a standardised format with elements in common between stations of a similar type. Find out more here.
For a more detailed guide on the recent MRCPsych exam changes, read our blog on Online MRCPsych Examinations.
Assessment Portfolio for Hong Kong Psychiatrists
The assessment portfolio should demonstrate achievement of equivalent competencies to those defined in the ARCP documented on the application form, including competencies in Psychotherapy AND Child and Adolescent Psychiatry, or Learning Disability, by the time of application.
In addition, you must demonstrate that you have undertake the following activities as part of your structured job plans:
Observation in interviewing patients in ward rounds for specified reasons
Observation in interviewing patients in out-patient or community settings or other contexts for specified reasons
Assessment via formal presentation of cases with their medical notes; discuss management of cases with their Clinical or Educational Supervisor
Formal assessment of competencies in Child and Adolescent Psychiatry or Learning Disability AND Psychotherapy
Assessments and achievement of competencies should take place in a range of settings and psychiatric specialties with structured, documented feedback on performance having been provided.
Whilst there is no assessment criteria form available, (this is incorporated into the online submission), take a look at the ARCP assessment portfolio form for CT1-3 in the UK, which should help give you a starting point for your own portfolio.
For Hong Kong Psychiatrists, the good news is that since the Hong Kong College of Psychiatrists embarked on the expansion and development of formal specialisms in psychiatry, the core competencies required by the Royal College in the UK are easier to gain access to than in other parts of the world. At the time of writing, the Hong Kong College oversees the following clinical divisions: general adult psychiatry, old age psychiatry, child and adolescent psychiatry, psychotherapy, addiction psychiatry, rehabilitation psychiatry and learning disability.
Postgraduate training in Hong Kong allows for MRCPsych aspirants to apply for the examinations with confidence.
Sponsorship Requirements
Hong Kong MRCPsych candidates must have a sponsor in place in order to support evidence that their three years of training satisfy Royal College criteria of having achieved equivalent competencies at appropriate competency levels (year 1, 2, 3) for each component of the examination.
Sponsorship is required by all applicants for entry to the CASC exam and your sponsor should be an appropriate medical education lead, confirming you have met the requirements to sit the MRCPsych examinations.
Acceptable sponsors in Hong Kong include:
College Tutor
Training Programme Director
Educational Supervisor
Head of School
Director of Medical Education (or equivalent)
Head of Department of Psychiatry
Consultant responsible for employee/trainee appraisal
Once your sponsor has authorised your application, you will receive a confirmation email from the Royal College, and you will be asked to complete your application and proceed to payment.
Applications for Hong Kong Doctors
To apply from Hong Kong, you will need to complete an online application form which takes about 15 – 20 minutes. Applications must be submitted no later than 3:30pm UK time (10:30pm HK time) on the last day of the application period.
Note: the online application form for Paper A, B and CASC will only be available during the published application dates and applications submitted after this will not be accepted.
You can sit Paper A and B in any order. You will be required to enter contact details and training history, including your medical registration. If applying for the CASC, you will also need to provide the contact details of your sponsor.
After you have completed the written exam, you have 1,643 days to sit the CASC – you can find specific time limits here.
Exam Costs and Payment
Payment is made by Visa or Mastercard credit/debit card, and the costs for 2021 are as follows:
Candidate
Paper A
Paper B
CASC
PMPT Trainees and Affiliates (UK & Ireland Centres)
£486 (~HK$5228)
£437 (~HK$4701)
£1,004 (~HK$10,799)
Non-PMPT Trainees and Affiliates (UK & Ireland Centres)
£539 (~HK$5797)
£485 (~HK$5217)
£1,115 (~HK$11,993)
Exam Locations
Due to the ongoing difficulties presented by the COVID-19 pandemic, the CASC examination will not be run in Hong Kong in 2022.
The good news is that changes have been made and all examinations for MRCPsych can be taken online. Hong Kong psychiatrists can now sit all three MRCPsych exams without leaving the country, and even from the comfort of your own home. This makes it easier for HK doctors to complete the MRCPsych examinations and work towards their GMC registration within a normal time frame.
Exam dates
These are the exam dates available at the time of writing.
Paper A
Diet
Date of Examination
Application Period
Publication of Results
2
8 December 2021
4 - 22 October 2021
11 February 2022
1
14 June 2022
4 – 14 April 2022
22 July 2022
2
6 December 2022
3 – 14 October 2022
15 February 2022
Paper B
Diet
Date of Examination
Application Period
Publication of Results
1
29 March 2022
25 January – 4 February 2022
13 May 2022
2
4 October 2022
25 July – 5 August 2022
4 November 2022
CASC - UK & Ireland
Diet
Date of Examination
Application Period
Publication of Results
1
10 – 21 January 2022
1 – 12 November 2021
25 February 2022
2
12 – 23 September 2022
6 – 17 June 2022
31 October 2022
How do I prepare for the MRCPsych examinations?
With lots of materials online, we have discussed with IMGs the best exam resources and materials for Hong Kong doctors. Most IMGs recommended starting with the Royal College, who have created useful resources to help you to prepare for the exams. See below:
Syllabus: We always suggest that this is the best place to start – plan your study around the curriculum topics and make a road map to your success in the exams. You can find this here.
Current critical review syllabus: For Paper B candidates will need to ensure that they make optimal use of the MRCPsych Paper B Critical Review Evidence Based Practice Syllabic Content.
Sample Papers: These will help you prepare and polish your exam techniques. They are helpful in familiarising yourself with the exam format to allow you to work quickly and efficiently on the day, and are a good way to benchmark your knowledge and progress against the syllabus.
Paper A sample questions
Paper B sample questions
Marking schemes (Paper A and B): Candidates pass or fail the written papers based on their performance, and not how well you perform against other candidates. As such, it is a good idea to understand how the exam is worked, so you can maximise your exam skills, giving you the best chance of a pass. Marking schemes can be found here.
Marking scheme (CASC): A good start with CASC preparation is to get to know how you will be assessed, take a look at the criteria for scoring a pass mark in CASC, as well as the History Marksheet, Management Marksheet and Examination Marksheet.
CASC examination guide: The Royal College have produced a helpful guide for candidates which provides information on stations, role plays and assessment.
CASC preparation videos: Here you will have the opportunity to see CASC stations in action. This will give you a good idea of what to expect and help you prepare.
CASC Blueprint: This helpful summary details stations in some detail and gives a useful overview of the exam format.
The Royal College also suggest taking a look at Passing the MRCPsych - an insider’s guide - a useful guide to help you to get over the first steps.
#IMG Tips
Start preparing early - as ever at IMG Connect, we believe in preparation. Early preparation gives you the best chance for success and lessens the need for the dreaded last-minute cramming.
Join a study group – a great way to share resources, tips and meet new friends at the same time! To join an international study group, get in touch on our Facebook community group, see below.
Practise, practise, practise – psychiatry IMGs preparing in Hong Kong have told us that it is vital that you practise your clinical examinations, even better if under the supervision of a colleague who has already passed the exams
Join the online psychiatry community – connect with like-minded psychiatrists and dedicated psychiatry recruiters in the IMG Psychiatrists Facebook group.
For regular news and updates on the Royal College and all things psychiatry, follow IMG Connect on social media using the links below:
Passed? What’s next?
Whether you completed MRCPsych as part of your postgraduate training some time ago, or have recently completed the examinations, you can apply for a full GMC registration with license to practice. Once the GMC has approved your application, you can work as a doctor in the UK.
This is a great time to get in touch with us to discuss your route towards and preparation for GMC registration, or to find psychiatry jobs in the NHS if you’re further along in the process. In the meantime, why not have a look at our blog on Finding Psychiatry Jobs in the UK for Hong Kong Doctors.
If you’ve passed part of the MRCPsych exams, it’s time to look ahead to your next exam. You can find comprehensive guides to each of the MRCPsych exams in the IMG Resources library.
A Microbiologist’s Route to the UK
There are several routes a microbiologist can take to register with the GMC and practice in the UK.
Microbiologists looking to secure a job in the NHS must satisfy certain criteria before to be eligible for GMC registration, which is a requirement to work in the UK. This generally depends on where you received your training, and the qualifications you hold.
In this blog, we’ll be giving you a snapshot of the steps you need to take to begin your journey to the UK as an overseas microbiologist. We’ll be covering the following:
What is the GMC?
What are the requirements for GMC registration?
How do I demonstrate my knowledge and skills as an EEA microbiologist?
How do I demonstrate my knowledge and skills as a non-EEA microbiologist?
How can I demonstrate my English language skills?
What is a certificate of good standing and how do I get one?
How do I register with the GMC?
Will I need a visa to work in the UK?
Skip ahead to the relevant section if you know what you’re looking for.
The General Medical Council
The GMC is the body in the UK which is responsible for licensing and revalidating every doctor. Therefore, for every doctor practicing in the UK, GMC registration is essential – you cannot practice in the UK without full GMC registration with a license to practise.
The primary responsibility of the General Medical Council is to ‘protect, promote and maintain the health and safety of the public’ in addition to improving medical education and practice across the UK.
Requirements for GMC Registration
Registering with the GMC is a multi-stage process, including key timings, actions and documents. For full GMC registration, international doctors must provide evidence of:
Skills & Knowledge for EEA Microbiologists
For microbiologists who trained in an EEA country (all countries inside the EU, also Lichtenstein, Iceland, Switzerland & Norway), you may be able to use your primary medical qualification (PMQ) or specialist qualification to register with the GMC.
Basic Medical Training
If you meet the requirements for basic medical training, you would be eligible for full registration.
You will not need to demonstrate your medical knowledge and skills to work as a doctor in the UK and would therefore not need to complete any additional skills and knowledge tests to register for a license to practice.
Specialist Training / Residency
If you meet the criteria for entry onto the Specialist Register, then once you have completed the GMC application process, you would be granted Specialist Registration in microbiology and can be appointed as a substantive or permanent consultant in the NHS.
Therefore, for European microbiologists, using your primary medical qualification (PMQ) or specialist qualification is most likely the easiest route to becoming GMC-registered and being able to practice microbiology in the UK.
To find out if your country’s qualifications will allow you to register for either GMC registration; check the relevant GMC page here.
If your training does not meet the GMC requirements for general or specialist registration, other routes you may consider to GMC registration as listed below.
Skills & Knowledge for non-EEA Microbiologists
If you qualified as a microbiologist outside the EEA, then you will have to demonstrate that both your medical knowledge and skills meet the level required to practice safely in the UK.
IMG microbiologists can demonstrate skills and knowledge through three main routes:
PLAB
PLAB or the Professional & Linguistics Assessment Board is a two-part exam that assesses a doctor’s ability to work safely as an SHO in the NHS, as such it does not demonstrate ability in microbiology specifically. For this reason, PLAB tends to be a route for junior doctors who have not already chosen their field of specialisation in medicine.
That said, for some senior doctors PLAB can be an attractive option, offering a quicker route to the UK, whilst still securing competitive salaries. If taking this option, microbiologists can then take up training or a more senior post once they have established themselves in the NHS. Take a look through our comprehensive guides on PLAB.
FRCPath Microbiology
The Royal College of Pathologists is the professional body that regulates the specialism of microbiology in the UK, and Fellowship of the Royal College of Pathologists (FRCPath) is the full qualification attainable by examination.
For overseas doctors, attaining FRCPath will satisfy the knowledge & skill criteria for GMC registration and facilitate application for more senior roles in UK pathology. Take a look at IMG Resources library for a complete guide to FRCPath to learn more.
GMC-recognised or equivalent qualifications
Some overseas qualifications and licensing exams are recognised by the GMC and accepted for registration purposes.
To find out if your qualification is accepted by the GMC, take a look at our blog: GMC-accepted postgraduate qualifications.
English Language Testing
Both EEA and non-EEA microbiologists, regardless of experience and country of origin, must demonstrate that they have a sufficient grasp and competence of the English language. This can be done by passing either the IELTS (International English Language Testing System) or the OET (OET – Occupational English Test). Detailed guides to these tests can be found below:
IELTS – a guide for overseas doctors
OET – a guide for overseas doctors
Exemption from English tests
For doctors who have at least two years of their most recent experience in an English-speaking country, you can use a reference from your current employer or employers over these two or more years to demonstrate competence of the English language. This would exempt you from sitting an English language exam.
Certificate of Good Standing
All doctors registering with the GMC must provide a certificate of good standing from each medical regulatory authority they’ve been registered or licensed with in the last five years.
The medical regulatory authority may send you a certificate of past good standing if you're not currently registered or licensed with them. You can find out which medical regulatory authority to contact via the GMC website here.
If there's no medical regulatory authority in the country to issue a certificate, the GMC will give you further advice once your application has been assessed.
Please note that each certificate is only valid for three months from the date it's signed and must be valid when we approve your application.
Applying for GMC Registration
Once you’ve completed your English language exam, you can now apply for full GMC registration with a license to practice. For registration, you must provide evidence of:
English language capabilities - either your IELTS, OET or an approved reference from your current employer
AND
Certificate of good standing – the certificate from your medical regulatory authority which demonstrates good standing
AND
(EEA microbiologists) Sufficient skill and knowledge – as an EEA microbiologist, this would either be your recognised EEA qualification
OR
(Non-EEA microbiologist) Sufficient skill and knowledge – as a non-EEA microbiologist, this would either be PLAB, FRCPath or a GMC-approved qualification.
To understand the registration process more fully, read our article on GMC registration for overseas doctors here.
Visas
IMGs relocating to the UK will need to apply for a visa from the Home Office.
A Tier 2 visa is the document given to a skilled worker by the UK Home Office following a job offer from a UK employer with a valid Tier 2 Sponsorship License. The list of valid Tier 2 Sponsors can be found here.
Understand Tier 2 visas and Certificates of Sponsorship in depth by taking a look at our article: Tier 2 Visa application process & documents needed.
Wondering whether you can relocate with your family? Take a look at our blog on the Tier 2 dependent visa below: Tier 2 Dependent visa - Can I bring my family with me to the UK?
There you have it! Hopefully this clarifies any worries or doubts you may have on your route to the UK as a microbiologist planning a career in the NHS. If you have any questions or wish to know more about the microbiology job market, then get in touch with our team.
For regular news and updates on the Royal College and all things pathology, follow IMG Connect on social media using the links below:
Route to CESR - Emergency Medicine Jobs
CESR acts as a route to applying for substantive (permanent) consultant jobs in Emergency Medicine for doctors who have not followed a specialty training programme in the United Kingdom.
In a nutshell it is the option available to emergency medicine doctors practicing as consultants, or at a senior level from overseas who wish to gain specialist registration in the UK. Some doctors choose to apply from overseas, others work with IMG Connect to secure a job in the NHS geared at helping them gain entry to the specialist register once in the UK.
If you are working as an Emergency Medicine consultant, or at a senior level in your home country and are eligible for specialist registration in the UK, then as an overseas doctor (IMG) you have a couple of options. Here we focus on applying for CESR from abroad as well as the alternative route, applying for a Specialty Doctor or Fixed Term Consultant job in the UK before applying for CESR with support of your NHS employer.
Both routes lead to gaining CESR and entry to the Specialist Register, meaning that you can work as a substantive consultant in the NHS. Both take hard work, preparation, evidence gathering, time and dedication. Both options have the same end goal, specialist registration.
It is important to say that no matter how you choose to apply, the CESR process involves submitting a large volume of evidence to demonstrate that you have the equivalent experience, skills and competencies as a doctor who has taken the specialty training route in the UK. Whether applying from overseas or not, some doctors are asked to complete additional experiences to meet this strict standard. Because of this, the process can be lengthy.
Applying for CESR from overseas
This is a great option for emergency medicine consultants who are not constrained by time and have an understanding department that will support the additional gathering of evidence.
The GMC reckons that it takes between 6 – 9 months between submitting your application and receiving a decision. At IMG Connect our experience tells us that is takes a similar amount of time to gather the evidence prior to submitting. In addition, you must have completed the evidence in the first place in real workplace and clinical scenarios. This can take twice as much time as preparing and submitting. Put simply, the process can be time consuming and laborious.
Add to this the issue of completing and gathering evidence against the CESR application from overseas. It can prove challenging to ensure that you have completed the full complement of competencies for CESR applications. This can result in the GMC asking for further evidence, adding more time to the process. You may have to identify gaps in your learning and then resolve them. It is not all bad though, this is good practice and will benefit you in the long run.
Applying for a specialty doctor job and/or fixed term consultant post before applying for CESR
For senior emergency medicine doctors who are keen to secure entry to the Specialist Register quickly, and work in the UK as soon as possible, then taking up a Specialty Doctor role with CESR programme, or a Fixed Term Consultant post with CESR programme/support is a good option.
Many NHS hospitals or trusts in the UK will offer access to support, clinical experience and study or preparation time for CESR. This is often built into the weekly job plan, but in some circumstances, this may be arranged informally. Either way, this is a good way for senior emergency medicine doctors to quickly gather the right evidence for their application with the support of their peers, senior colleagues and NHS employer. This can shorten the time spent on the application overall.
If this sounds like the best option for you, it is wise to start gathering and signing off evidence in your current consultant post. That way you will already have some or most of the required evidence for CESR in place, allowing you to quickly focus on any elements that are missing once in the UK and working in the NHS
Find an emergency medicine job in the NHS with CESR
Securing a job as a Specialty Doctor with CESR programme attached, or a job as a Fixed Term Consultant with CESR programme/support attached, gives you instant exposure to the UK system, NHS experience and a great start to your career in the NHS.
To discuss whether applying for CESR from overseas or securing a job as a Specialty Doctor or Fixed term consultant with CESR programme is the right route for you towards specialist registration, speak with an IMG Connect consultant, register or send your CV.
IMG Jobs
Search and find live emergency medicine NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor jobs, doctor salary & relocation for emergency medicine specialists
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss emergency medicine doctor job options in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.
For the latest news and updates on all things emergency medicine, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.

FRCR Part 1 – a detailed guide for international radiologists
FRCR Part 1 or CR1 is the first exam in the FRCR postgraduate qualification.
The completion of all the exams in the Fellowship of the Royal College of Radiologists (FRCR) examination suite leads to eligibility for GMC registration. The exams can be taken by IMGs from any country, provided certain criteria have been met. In this article, we’ll take a look at the following:
An overview of FRCR exams
A deep dive into FRCR Part 1
How is the exam marked?
Am I eligible for the exam?
As an overseas radiologist, where can I sit the exam?
How much will the exam cost and how do I apply?
What is the best way to prepare for the exam?
#IMG Tips
I’ve passed the FRCR Part 1 exam, what’s next?
Skip ahead to the relevant section if you know what you’re looking for.
An Overview of FRCR
FRCR is the set of postgraduate examinations administered by the Royal College of Radiologists to test a candidate’s knowledge and clinical understanding within the scope of the Specialty Training Curriculum for Clinical Radiology.
The exams are as follows:
Please note that only full FRCR satisfies the postgraduate requirements for overseas doctors.
You can read an overview of the full FRCR examination suite via our IMG Resources library.
For doctors who are interested in securing senior roles in the NHS which are reflective of their current practice or grade, we advise that FRCR is the best route to take to GMC registration. FRCR is often a requirement for NHS locum consultant job postings where candidates are not already on the Specialist Register for radiology. The FRCR route allows senior candidates to better align their qualifications with the specifications of relevant jobs.
FRCR Part 1 - Anatomy & Physics
FRCR Part 1 is the first in the set of FRCR exams. This exam expects candidates to have gained knowledge of the physical principles that underpin diagnostic medical imaging and of the anatomy needed to perform and interpret radiological studies.
The exam is designed to assess whether candidates have an appropriate knowledge of the anatomy that underpins all radiological imaging including radiography, fluoroscopy, angiography, computed tomography (CT), ultrasound imaging and magnetic resonance imaging (MRI).
The two components of the exam are Anatomy and Physics.
Anatomy
The exam features an electronic image viewing session, mimicking what radiologists would encounter in clinical practice in order to be valid, thus the questions consist of radiological images on a computer screen as this is the normal medium, as opposed to film or printed on paper.
The exam includes 100 questions - most of these are quite straightforward with an arrow indicating a specific anatomical structure as shown by a specific modality. These are typically “name the arrowed structure” questions, with space provided for a free text answer.
The exam lasts 90 minutes and individual modalities are given roughly equal weight as follows:
cross-sectional
plain radiographs
contrast studies
Different body parts are also given roughly equal weight covering the following areas:
head, neck and spine
chest and cardiovascular
abdomen and pelvis
musculoskeletal
Recognising a radiological anatomical structure and unprompted recall of its precise name is a key aspect of the everyday work of clinical radiologists, and doing so in a timely manner without routine recourse to reference material reflects real-life clinical practice.
Physics
The purpose of the physics exam is to assess whether candidates understand the underlying principles that underpin the generation of images in the various modalities, such that they:
select the most appropriate imaging technique for a clinical scenario from the intrinsic properties of the method of image generation
understand the risk, safety and quality consideration that are inherent in image generation to allow an informed choice of the appropriate modality and any alteration in technique
demonstrate the requirements of legislation that require the use of those techniques that require ionising radiation to be justified by a professional had been met
This exam lasts two hours and comprises 40 questions. Each question includes a stem (a question or statement) and five items (answers). The answers must be marked true or false and it is possible for all five items to be true or for all to be false.
The question distribution of the physics paper is as follows:
matter and radiation – 3
radiography & fluoroscopy – 6
radionuclide imaging – 6
radiation safety – 6
computed tomography – 6
magnetic resonance imaging – 6
ultrasound – 6
other – 1
Marking
Both exams are marked by a delivery platform which is programmed with the correct answers.
Marks are awarded for each exam as follows:
The anatomy examination is marked out of 200, and answers are marked as follows:
full accuracy = 2 marks
less accuracy, but still correct (e.g. omits ‘left’ or ‘right’ for a paired structure) = 1 mark
incorrect = 0 marks
The physics examination is marked out of 40, and answers are marked as follows:
correct = 1 mark
incorrect = 0 marks
The standard for success is determined based on the difficulty of the questions in each sitting and may therefore vary between sittings and sets of images.
For more information on the exam content and structure, read the guidance notes for candidates on the College website.
Eligibility
The eligibility criteria for FRCR Part 1 is:
holding a Primary Medical Qualification (PMQ) that is recognised by the GMC for registration purposes.
holding a formal clinical radiology post in which they are actively receiving clinical radiology training.
no minimum period of clinical experience or training is required to enter the exams
Exam Centres
The current venues for the First FRCR (CR1) exam are:
Belfast, Birmingham, Bridgend Wales, Crewe, Edinburgh, Glasgow, Leeds, London and Plymouth. Overseas centres for now are in Hong Kong, Singapore, India, Egypt and Malta.
The exam is typically held three times a year over two consecutive days. 2023 exam dates are as follows:
February 2023
Physics – Thursday 9 February
Anatomy – Friday 10 February
June 2023
Physics – Thursday 8 June
Anatomy – Friday 9 June
September 2023
Physics – Thursday 14 September
Anatomy – Friday 15 September
For updates on exam dates, including the application window, keep an eye on the Royal College website here.
Applications & Cost
First FRCR (CR1) 2023 exam cost:
Members - £319
Non-members - £406
Please note that these costs vary slightly for some overseas centres.
UK trainees are given priority for examination places, followed by members of the Royal College and finally non-members. Each window lasts around a week and all candidates should apply for the exams through the Royal College website here.
Preparation
Although there are many online materials to aid in your preparation for FRCR Part 1, as always, we recommend you start your preparation on the Royal College website, particularly with the Specialty Training Curriculum for Clinical Radiology. In using these as a blueprint for your preparation, you will ensure your study is focused on the most relevant and useful information as prescribed directly from teaching materials.
Instructional video and demonstration site: a walkthrough video of the FRCR Part 1 exam format with guidance and instructions which can be found here for the physics component and here for anatomy.
Anatomy module guidance: advice for the anatomy module has been compiled by the College here.
Specimen questions: sample questions and answers have been put together by the College and are available here.
#IMG Tips
Prepare early – the best way to avoid stress and last-minute cramming is to get started as soon as possible.
Get familiar with the exam content – during your study (at least to start off with), the curriculum should be your guide to the FRCR exams.
Practise, practise, practise – go through as many practice questions as you can and regularly review your progress using mock exams.
Sources
https://www.rcr.ac.uk/clinical-radiology/examinations/frcr-part-1-radiology-cr1
https://www.rcr.ac.uk/sites/default/files/cr1_anatomy_purpose_of_assessment_statement.pdf
https://www.rcr.ac.uk/sites/default/files/cr1_physics_purpose_of_assessment_statement.pdf
https://www.rcr.ac.uk/sites/default/files/clinical_radiology_curriculum_2020.pdf
I’ve passed the First FRCR exam, what’s next?
Firstly, congratulations! This is an incredible achievement, and you deserve to treat yourself after all that hard work! With a pass in the First FRCR in hand, you can look ahead to the Final FRCR CR2A and CR2B exams. Once you have completed all parts of FRCR, you can apply for full GMC registration with a license to practice.
Don’t hesitate to get in touch with our team to learn more about the opportunities available to you once you’ve passed FRCR.
For the latest news and updates on all things radiology, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.
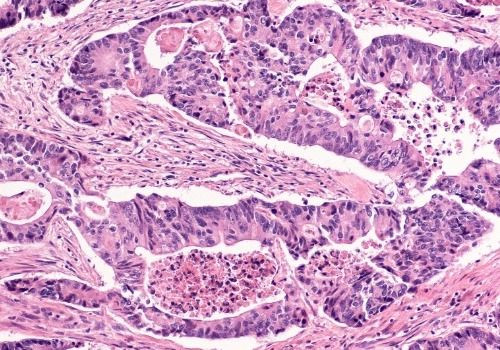
Histopathology Jobs in the UK – a guide for Hong Kong pathologists
Are you a histopathologist from Hong Kong looking to live and work in the UK? Do you want to know how to find the best jobs for overseas pathologists in the NHS?
With recent experience of working with Hong Kong Pathologists on their journey to the UK, we thought that we’d share a few snippets of information to help get you started.
In this blog we will cover the following topics:
What do Hong Kong doctors need to work in the UK?
As a Hong Kong pathologist, will I fit into the NHS?
What kind of jobs can I find in the UK?
Where can I find NHS jobs in histopathology?
Can I get access to CESR?
What if I don’t have FRCPath Histopathology?
How do I register with the GMC?
What visa will I need to work in the UK? BNO or Tier 2?
Getting started
Skip ahead to the relevant section if you know what you’re looking for.
Requirements to work in the UK
To be eligible to work in the NHS, histopathologists from Hong Kong must have full GMC registration – this requires completion of the Royal College of Pathologists exams in the relevant specialty I.e. histopathology (FRCPath), as well as an English language exam and Certificate of Good Standing (CGS).
From our experience, the majority of Hong Kongers are either aware of the UK Royal College exams or have already completed these as part of their specialist pathology training, so great news - you are more than likely already halfway there!
If you are unsure about the requirements for FRCPath, you can find an overview of FRCPath Histopathology here.
How Hong Kong Pathologists fit into the NHS
Pathologists from Hong Kong are a great fit for the NHS. And no matter your specialist training or sub-specialty interest in within histopathology, our NHS clients would consider you to be a high calibre candidate. Why? The training in Hong Kong is thorough and highly regarded here in the UK among NHS clients.
If you are not sure about how your experience will translate to working in the NHS, then we are here to help - IMG Connect are experienced working with all areas of sub-specialty within pathology, across all major organ sites.
Senior Histopathology Jobs in the NHS
This all depends on the experience and qualifications you gained in Hong Kong. Whilst there are a lot of similarities between our two healthcare systems, there are also a lot of differences too.
Attaining full FRCPath demonstrates the ability to report on cases and as such typically qualifies candidates to work independently as consultants in the UK. Think of it as like the FHKCPath and the accompanying Fellowship of FHKAM (Pathology) examinations.
NHS clients will look out for your experience and training combined with this postgraduate qualification in order to work out what level you will start at.
For consultant histopathologists who have already completed their anatomical pathology specialist training in Hong Kong, you will most likely enter the NHS as a locum consultant or in other senior positions such as Specialty Doctor (SAS), or Specialist Grade. This is generally up to the NHS Client, although, if starting in a specialist position, the aim here is that you will receive support to acclimatise to the UK system, in order to quickly work towards a consultant post. This will be agreed before your arrival in the UK.
There is demand in all areas of histopathology, particularly at the consultant level. So, it is important to understand where you fit into the NHS, and we would be delighted to guide you through the process. Send in your CV or register with us through the buttons above or below, and we will arrange an informal chat with you to discuss your job options in full.
Finding NHS Histopathology Jobs
You can get full access to the most recent histopathology job postings straight to your inbox through IMG Connect.
The latest NHS pathology jobs cover general histopathology and cytology, as well as a number specialised or part-specialised posts where you may report one anatomical area extensively, or perhaps 2-3 areas. With just a few clicks, you can create an account and customise job preferences to receive email alerts on job that suit your professional and personal needs.
Sign up here to receive up-to-date information on NHS jobs which you can tailor to your job preferences and receive straight to your inbox.
CESR for Hong Kong Pathologists
As the UK FRCPath qualification is not commonly taken during the Hong Kong residency programme, CESR presents itself as a more favourable option for some.
CESR is a big process that involves submitting around 800 - 1000 pages of verified evidence that you’ll need to gather from the last 5-6 years of clinical practice, either in the UK or overseas.
Given the Hong Kong Royal College of Pathologists' curriculum is so closely aligned with the UK’s Royal College, pathologists from Hong Kong are actually some of the best primed to attain Specialist Registration via CESR, without working in the UK first.
Whether it’s quicker to complete FRCPath, or to prepare a CESR application directly from Hong Kong, entirely depends on your background and experience. With that in mind, if you want to understand more, please send across a copy of your CV to our team and we can talk you through your options.
For a detailed guide on CESR for histopathologists, see our IMG Resources library.
Routes to the UK for Hong Kong Pathologists
The standard test of knowledge in the Histopathology curriculum in the UK is FRCPath Histopathology, although you do not need this to register with the GMC.
There are four main routes to the UK for Hong Kong pathologists:
The differences between these routes can be best understood through our explainer blog here.
Essentially, whilst FRCPath can be more time-consuming and expensive than other routes, our advice is that it is well and truly worth the investment – histopathology is a consultant-led specialty in the UK and therefore FRCPath Histopathology opens up many more opportunities (particularly for more experienced pathologists) than alternatives such as PLAB or Sponsorship.
Clients look out for FRCPath, and combined with your experience, this will move your CV to the top of the pile.
As discussed above, although Hong Kong histopathology training is well aligned with the UK system, CESR can either be an easier or more arduous route to GMC Registration depending on your level of experience.
Remember however:
CESR = Specialist Registration and FRCPath = General Registration
If you would like to pursue the CESR route and would like to know more about pathology jobs that offer CESR support, do get in touch.
If you are just beginning your journey through the FRCPath Histopathology exams, please see our blog here for an overview of the exams.
We also have an online IMG Histopathologists community on Facebook which as well as providing support and resources on FRCPath, also offers guidance on GMC registration and other aspects of relocating to and working in the UK.
How to Register with the GMC
Once all the necessary components for GMC registration have been completed, Hong Kong IMGs can then apply for full GMC registration with license to practice.
There are further checks involved in the registration process, such as verification of medical degrees, however these are steps that will be taken care of with your IMG Connect recruitment specialist.
However, if you’d like to learn more about these processes, you can find information in our blog breaking down the steps to GMC registration for overseas doctors here.
Visas for Hong Kong Doctors
Honk Kong residents with British National (overseas) status can apply to travel to the UK to live for up to five years with dependent family members, through the British National (Overseas) visa.
You also have the option of securing a Skilled Worker visa, or Health & Care visa to give the most recent term. We know that securing a visa in Hong Kong can be challenging at the moment, so if you think that the Health & Care Visa is a good option for you, don’t hesitate to connect with us to discuss your options.
For a detailed guide to your visa options as a Hong Kong doctor, you can read our blog discussing the differences between the Tier 2 Skilled Worker and BNO visas here.
Getting started
We are here to help with all questions, big or small, whether you are starting out on your journey or ready to look explore jobs. Register below or get in touch to speak with one of our dedicated histopathology recruiters.
We hope this helps and wish you the best of luck in your search!
To receive the latest news and updates on all things histopathology, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation:

MRCP (UK) PACES - What if I can't secure an exam place?
Exam places for MRCP PACES have been hard to secure in some countries. This increase in demand has continued through to 2023, so what can you do to maximise your chances of securing an examination place?
The Royal College of Physicians has advised that they are working to grow capacity internationally. However, this will not have an immediate impact on the number of spots available across the world.
With so many overseas doctors missing out on a spot, we have put together some of the main discussion points to help you to broaden your chances of sitting the exam as soon as possible.
All applications submitted during the application period will be treated equally, with spaces being allocated using a random lottery model. Some spaces are reserved for local trainees and some priority can be given for applicants near the end of their eligibility periods.
So, to maximise your chance of success, we suggest that not only do you apply to your closest PACES exam centre, but also to 3 more centres that you are able to travel to.
Apply to more centres
Why should I apply for more centres? More applications equals more chance of securing a place. They way that it works is that if you are not successful with your 1st preference (most local centre), then you will be considered for a space in your 2nd choice centre, and so on until you secure a spot.
Of course, this means that you must be willing to travel to sit the exam. This can be costly, especially if you have to travel to a different country, flights and hotels are not cheap! As such, we suggest taking some time to carefully choose the locations that will not only have the possibility of a spare place, but where your costs will be kept to a minimum.
Candidates will be notified on the outcome of their application within 2 weeks from the closing date, giving you time to plan your travel if necessary.
Whilst this advice does not guarantee a place to sit the exam, it will increase your chances.
If you are not sure what to do, or have any other questions regarding the PACES exam, get in touch with an IMG Connect specialist.
Take a look at our IMG library for more information regarding postgraduate exams & PACES
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss doctor job options in the NHS, including discussions regarding CESR, a typical doctor salary in the UK and the most suitable NHS jobs & hospital locations for you.
Follow us on social media for news and updates on GMC registration, the Royal College and NHS through the links below:

IMG Connect’s 7 Top Tips for exam preparation
As an overseas doctor, preparing for your royal college or PLAB exams can be a daunting prospect and requires a huge amount of learning. IMGs have told us that the top tips below helped them improve their scores on their journey to exam success.
1. Find a study group or partner
For a lot of people, studying with others is both motivational and more sustainable.
Whether to share exam tips, test each other or just be there for a bit of emotional support – the benefits are endless. Oh, and it’s free!
2. Join an online community
By joining online communities of doctors in similar positions, you will surround yourself with people in the same position, revising the same topics and preparing for the same exams. Just like having a study group or partner, this can offer you a huge support network and won’t cost you a penny!
3. Use the internet to its full potential
There are lots of very useful content, for all exams, available online & free of charge. Whether you’re taking an English Language test or a postgraduate exam, someone will have created an online resource for you. From podcasts and YouTube videos, to reading materials, curriculums & study guides - make sure you are using the internet to its full potential!
Ask your study groups, partner or online community which resources have worked well for them.
4. Use the GMC and your Royal College to their full potential
Similarly, the GMC or your Royal College will usually have lots of useful links and documents to help you prepare. Have a look online and use all of them where you can, we have tried to highlight them throughout our blogs to help you make a start.
5. Courses & Study Books
Whilst you don’t necessarily have to pay for courses and books to aid your studies – most IMGs have found substantial benefits in using them. Do your research and ask those around you what has worked well for them.
6. Don’t burn out
Avoid leaving everything to the last minute and make sure you stay healthy and sleep properly during your preparations. Whilst these exams are of course very important, don’t burn yourself out at the cost of good rest. You might consider yourself a night owl but your productivity will plummet without a good night’s sleep.
7. Plan your studies & staying ahead
Take the time to get to know your syllabus as early as possible and use it as a road map for your study plan.
Once you have your plan, stay on top it and try and get ahead – you don’t want to be cramming revision in at the last minute at the cost of your day-to-day life.
Join our IMG Community, if you haven’t already done so
The IMG Community is an open group that provides an informed & regulated platform for any doctor to ask questions and share their experiences. The focus of our business is to help doctors find work and relocate to the UK, and IMG Connect proves to be an effective way of managing this process for you.
From answering any questions on your:
exams
registrations
qualifications
To providing planning & support with:
relocation
integration with your local community
schooling
ongoing career support
Remember, both our platform and our service are free of charge from start to finish.
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss doctor job options in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.
For regular news and updates, follow IMG Connect on social media using the links below:

MRCEM vs PLAB - GMC Registration for Emergency Medicine IMGs
GMC Registration can be a long and complex process. With several options available for overseas doctors to demonstrate evidence of their skills and knowledge, it might be difficult to decide the best route to take to register with the GMC.
For international doctors planning their route to the UK, the two most common and popular routes by far are the UK postgraduate qualifications (MRCEM for emergency medicine physicians) or PLAB. Here we provide a summary of both pathways and briefly consider their benefits to help you make the best choice in your journey to the UK as an IMG.
GMC Registration for Overseas Doctors
PLAB for GMC Registration
MRCEM for GMC Registration
Which is better for me as an IMG: PLAB or MRCEM?
#IMG Tips
How do I get started?
Skip ahead to the relevant section if you know what you’re looking for.
GMC Registration for Overseas Doctors
Registering with the GMC is a multi-stage process, including key timings actions and documents. To receive full registration, international doctors must provide evidence of:
What is often the most long and challenging part of the process is providing sufficient evidence of skills and knowledge, however, you can check whether you have a GMC-accepted postgraduate qualification here.
There are 5 ways in which an overseas doctor can demonstrate their skills and knowledge:
PLAB
Acceptable Postgraduate Qualification / Licensing Examination
Relevant European Qualification
Sponsorship / MTI
CESR / CESR-CP / CEGPR
Please note that only one type of evidence is required to demonstrate skills and knowledge for GMC registration.
Of these routes, the most accessible are PLAB and the Acceptable Postgraduate Qualification because they are two of the only routes that do not depend on the country you’ve trained in – the UK postgraduate exams and PLAB can be sat by doctors.
For a detailed breakdown of all the routes available to IMGs, see our blog here.
PLAB - Professional & Linguistics Assessment Board
The first and most common route we’ll be discussing, which is particularly popular among junior doctors, is PLAB.
PLAB is a two-part exam (one written and one practical element), which assesses whether a candidate is at least as capable as a doctor starting the second year of their Foundation Programme Training (FY2 or F2) and can therefore work safely as an SHO (Senior House Officer) in the NHS.
The GMC has produced a useful video summary of the PLAB exams which you can watch here, or for a more detailed overview, see our IMG Resources library.
MRCEM - UK Postgraduate Qualification for Emergency Medicine
The UK’s postgraduate qualifications are a more popular route for senior overseas doctors, and those looking to gain posts in the NHS which are reflective of their experience.
For emergency medicine, this can be done by attaining Membership of the Royal College of Emergency Medicine. The Royal College of Emergency Medicine (RCEM) is the professional body that regulates the specialism of emergency medicine in the UK, and Membership of the College of the Royal College of Emergency Medicine (MRCEM) is the full qualification attained through these examinations.
Take a look at our IMG Resources library for complete guides on MRCEM to learn more.
You can also read our interview with Dr Behzad Rashid to learn about the experience of an IMG Emergency Medicine resident going through MRCEM.
PLAB vs MRCEM
Both MRCEM and PLAB are respectable routes that demonstrate skills and knowledge and will allow an international doctor to register with the GMC and work in the UK. To decide which route of the two is best for you, you’ll need to consider the benefits of each and how they align with your needs and priorities in moving to the UK.
Seniority of Positions in the NHS
It would be difficult for an overseas emergency medicine doctor to obtain a more senior post in the NHS without either MRCEM, a GMC-approved training programme, or extensive experience from a similar English-speaking healthcare system. PLAB alone will not give overseas doctors access to senior posts in the NHS.
Training
To practice as a consultant in the UK, you must have gone through specialty training and will need a GMC-recognised postgraduate qualification to do so, whether a qualification from the country in which you completed your specialty training, or MRCEM.
Due to the more specialised nature of MRCEM, we advise emergency medicine doctors to complete MRCEM, as many NHS Trusts will list MRCEM as a requirement on job descriptions. MRCEM also allows IMGs access to more senior roles and competitive salaries.
Time
PLAB has two stages and can take anywhere between 3-9 months to prepare from start to finish.
MRCEM has three stages, the last of which must be taken after at least 24 months of postgraduate experience with at least 6 months in emergency medicine and can take anywhere between 24-36 months to prepare from start to finish.
Cost
MRCEM costs £1,115 for the three exams. Whilst the Primary and Intermediate SBA exams are delivered worldwide via computer-based testing company, the OSCE is delivered in London (UK), Kuala Lumpur (Malaysia), Chennai, Hyderabad, Mumbai and Kochi (India), so there may be the added expense of international travel.
PLAB costs £1,189, and whilst PLAB 1 can be sat in many overseas centres around the world, PLAB 2 is only delivered in the UK. You can find a list of overseas centres for PLAB 2 here.
So for both MRCEM and PLAB, candidates will have to travel to the UK, meaning that the additional cost of visas, accommodation and flights must be factored in.
It’s also important to note that these costs can rise if re-sits of the exams are necessary.
Summary
PLAB, as an exam which examines a doctor’s ability to work safely as an SHO, does not assess ability in emergency medicine specifically. For this reason, PLAB tends to be a route for junior doctors who have not already chosen their field of specialisation in medicine, I.e., emergency medicine.
PLAB allows doctors to enter the UK system much faster than other routes and for this reason alone, it is favoured by international doctors when considering their path to the UK.
MRCEM involves three more difficult examinations and takes more time to prepare for. However, for overseas doctors, attaining MRCEM will allow you to jumpstart your career in the UK, as you don't need PLAB or Core Training.
Additionally, MRCEM will facilitate the application for more senior roles in UK emergency medicine than PLAB.
#IMG Tips
Determine your priorities – your goals and timeline for relocating to the UK are important in deciding which route is best for, and this is different for everyone.
Plan well ahead – depending on the route you choose, you may be embarking on a long journey through these exams, so plan how you will fit them into your life and how best to prepare to maintain a good work-life balance at the same time.
Find a support network – once you know which exams you will sit, find a support network of others who are also preparing for the exam.
Sources
https://rcem.ac.uk/exam-mrcem/
https://www.gmc-uk.org/registration-and-licensing/join-the-register/plab
https://www.gmc-uk.org/registration-and-licensing/join-the-register/before-you-apply/evidence-to-support-your-application
Getting started
Once you’ve decided which exams are best for you, it’s time to delve deeper into the exams and what they entail. For more useful blogs and articles on PLAB or MRCEM, registrations and qualifications to help you find your dream job in the NHS - take a look at our IMG Resources library.
Don’t hesitate to get in touch with one our recruitment specialists if you would like to discuss your options in the NHS once you have completed PLAB or MRCEM.
For the latest news and updates on all things emergency medicine, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.

Final FRCR Radiology (Part 2A & 2B) - a guide for IMGs
FRCR CR2A and CR2B and the final exams in the FRCR qualification.
Completions of all three parts of the Fellowship of the Royal College of Radiologists (FRCR) qualification results in eligibility for GMC registration, once the English language component has also been met.
The FRCR examinations are key to an international oncologist being able to secure senior oncology jobs in the NHS and can be taken by IMGs from any country, provided certain eligibility criteria have been met. In this article, we take a closer look at the following:
An overview of FRCR
How are the Final FRCR exams structured?
How are marks awarded for CR2A and CR2B?
Am I eligible to sit Final FRCR?
Where can I sit the exams and how much do they cost?
How do I apply for the exams?
What is the best way to prepare for FRCR CR2A and CR2B?
I’ve passed the FRCR Radiology exams, what’s next?
Skip ahead to the relevant section if you know what you’re looking for.
An Overview of FRCR Radiology
FRCR Radiology is the set of three postgraduate examinations administered by the Royal College of Radiologists to test candidates’ knowledge and clinical understanding within the scope of the Specialty Training Curriculum for Clinical Radiology.
The exams within the exam suite are as follows:
You can read an overview of the full FRCR Radiology examination suite via our IMG Resources library.
Please note that only full FRCR satisfies the postgraduate requirements for overseas doctors.
Alternative routes to GMC registration include PLAB and other recognised GMC qualifications or licensing exams, which you can find out more about here.
A Deep Dive into FRCR Part 2A & 2B
Final FRCR Part A
The Final FRCR Part A examination assesses knowledge of the sciences that underpin clinical radiology including physics as applied to imaging including molecular biology, medical statistics, radiological findings in pathological and normal conditions together with their differential diagnosis, management pathways, and radiological interventions.
The examination comprises two single best answer papers, each containing 120 questions and covering a broad range of the core curriculum. Exams are 3 hours for each sitting.
The paper comprises a mix of questions from across a wide range of the curriculum:
Cardiothoracic and Vascular
Musculoskeletal and Trauma
Gastro-intestinal
Genito-urinary, Adrenal, Obstetrics & Gynaecology and Breast Paediatric
Central Nervous and Head & Neck
Final FRCR Part B
The Final FRCR Part B examination assesses different aspects of a candidate’s radiological skills, all of which are considered necessary for safe and effective radiological practice.
The exam has three components:
reporting (long cases) – 6 cases in 75 minutes
rapid reporting – 30 plain radiographs in 35 minutes
oral exam – 2 x 30-minutes vivas
The stations are broken down in more detail below.
Reporting Station
This component is built on the fact that A&E department is a large part a radiologist’s workload.
The station tests candidates’ ability to rapidly decide if an image is normal or abnormal and the provision of a diagnosis for the abnormality.
The images are all radiographs with the balance of normals within the images about 45-50%. Trauma cases are the majority, but some chest and abdominal radiographs are included as they would be in a typical session of A&E reporting in the workplace. Each abnormal case shows one significant diagnosable abnormality.
This part of the examination reproduces the situation of plain film reporting as a safe radiologist needs to be able to identify abnormalities when present and confidently exclude them when they aren’t.
Rapid Reporting Station
The reporting component centres around the understanding that radiologists largely communicate their findings through written reports.
This element tests the ability of the candidate to make observations, distinguish the relevance of these findings, deduce a list of differential diagnoses, suggest the most likely diagnosis and discuss further management including further imaging where appropriate.
This part of the examination mirrors a mixed list of cross-sectional and fluoroscopic imaging, and a short, structured reporting sheet is provided. Each case can include any type of radiological imaging and often involves more than one e.g. plain film, CT and isotope study.
This written element of the examination aims to test the candidate’s ability to assess and interpret a variety of clinical cases across all modalities safely, and to accurately communicate their findings, conclusions and recommendations.
Oral Examination
This mirrors the day-to-day clinical discussions and MDT meetings, which form an integral part of a radiologist’s workload.
The oral component further assesses the candidate’s powers of observation and interpretation, but in addition allows assessment of the candidate’s ability to discuss wide-ranging aspects of patient care as influenced by the radiological findings.
Candidates are expected to be able to integrate their observations with emerging clinical information to help refine their differential diagnosis. It also tests their ability to communicate effectively, their analytical and decision-making skills, and allows searching questions to explore their depth of knowledge and ensure that their practice supports patient safety.
This oral element aims to explore the candidates’ depth of knowledge and to test higher cognitive skills. The format allows for flexibility and for complexity to be built into the examiner’s questioning.
In total, the Final FRCR exam lasts 2 hours and 50 minutes.
Scoring
Final FRCR Part A
The examination is marked by the examination software Speedwell and the marking system shown below is used:
For each item correctly answered: +1 mark
For each item incorrectly answered: 0 marks
The examination is not negatively marked and therefore you are encouraged to provide an answer to all the questions.
You can find full information on the scoring system for the CR2A exam here.
Final FRCR Part B
Reporting
Eight marks are available for each case, with a maximum of 48 marks available.
Candidate response
Mark
Excellent: a perfect answer, clear and confident
8
Good Pass: additional relevant material included in a "pass" grade answer
7
Pass: most observations made correctly; principal diagnoses correct
6
Borderline: appropriate for cases with two main diagnoses, but only one is mentioned; some observations missed
5
Fail: significant observations missed; correct diagnosis not made
4
No answer offered
3
Half marks may also be awarded.
Following the marking exercise each candidate will have a score between 18-48. An overall reporting mark is then awarded on the basis of total marks achieved using the scale below:
Total marks
Overall mark
18 - 25
4
25½ - 28
4½
28½ - 31
5
31½ - 34
5½
34½ - 37
6
37½ - 40
6½
40½ - 43
7
43½ - 46
7½
46½ - 48
8
Rapid reporting
One mark is available per image, with a maximum of 30 marks available.
Image type
Candidate response
Mark
Normal Image
Correctly classified
+1
Incorrectly classified (appropriate false positive)
+½
No answer given
0
Abnormal Image
Correctly classified and correctly identified
+1
Correctly classified but incorrectly identified
0
Incorrectly classified (false negative)
0
No answer given
0
Following this, each candidate will have a score between 0-30. An overall rapid reporting mark is then awarded on the basis of total marks achieved using the scale below:
Total marks
Overall mark
0 - 24
4
24½
4½
25 - 25½
5
26 - 26½
5½
27
6
27½ - 28
6½
28½ - 29
7
29½
7½
30
8
Oral
Candidates are shown images by two pairs of examiners and can score a maximum of eight marks from each pair.
Performance description
Comments
Score
Very Poor Answer
Key findings missed even with help
Wrong or dangerous diagnosis
4
Poor Answer
Slow to spot abnormality
Poor differential diagnosis
Needed help to get correct answer
5
Principal findings seen
Some abnormalities seen with help
Principal diagnosis correct
Limited differential
6
Good Answer
Key findings spotted quickly
Correct deductions made and correct diagnosis
Good differential offered
7
Excellent answer – all findings seen
Correct diagnosis and deductions
No errors
Succinct/accurate report
Excellent differential
8
Overall Pass Mark
Once the marks have been combined, each candidate will have a score of 4-8 in each component of the examination (two orals, the reporting session and the rapid reporting session).
The pass mark in each component is 6, making the overall pass mark 24.
In addition, candidates must obtain a mark of 6 or above in a minimum of two of the four components. If a candidate scores less than 6 in three or more components, they fail the examination even if they have achieved a score of at least 24 overall.
You can find full information on the scoring system for the CR2B exam here.
Eligibility for Final FRCR
Final FRCR Part A - to be eligible you must:
have passed FRCR Part 1
Final FRCR Part B - to be eligible you must:
have passed FRCR Part 1
have passed FRCR Part 2A
have acquired 34 months in a formal clinical radiology training post by the month of the examination (your training supervisor must provide confirmation that you have completed the required duration of training and received instruction covering the examination syllabus)
Exam Fees & Venues
Part 2A
The Part 2A exam is held twice a year, normally in spring and autumn.
You can see a breakdown of the fees for all UK and overseas centres below:
UK
Venues
Member fee
Non-member fee
Belfast, Bridgend Wales, Crewe, Edinburgh, Glasgow, Leeds, London, Plymouth
£427
£545
Global
Venues
Member fee
Non-member fee
Egypt
£427
£545
Hong Kong
£427
£545
India
£505
£643
Pakistan
£427
£545
Singapore
£493
£628
Part 2B
The Part 2B exam is now held four times a year.
You can see a breakdown of the fees for all UK and overseas centres below:
UK
Venues
Member fee
Non-member fee
Belfast, Bridgend Wales, Crewe, Edinburgh, Leeds, London, Plymouth
£597
£759
Global
Venues
Member fee
Non-member fee
Egypt
£427
£545
India
£505
£643
Applications
Applications are normally open for a few weeks, several months before the exam. Please refer to the examinations page for up-to-date information on application dates.
UK trainees (members) are given priority for examination places, followed by other member bookings and finally non-members. The window for each group is usually open for around a week before it opens to the next group.
All candidates should apply for the exams through the Royal College website here for Part 2A and here for Part 2B. More detailed information can also be found here in relation to preparation for the application.
Preparation
There are many resources available online to aid in preparation for the FRCR Part 2A and 2B exams. We always recommend that the best place to start your preparation is the Specialty Training Curriculum for Clinical Radiology.
Using this as a blueprint for your preparation is the best way to ensure your study is focused on the most relevant and useful information as prescribed directly from teaching materials.
Other useful resources to aid your studies include:
Instructional video: demonstrations of both parts of FRCR Part 2, providing insight into both elements of the exam and what candidates can expect on the day. These are on the RCR website here.
Guidance notes for Part 2A: a guidance document on key elements of the exam, found here.
Guidance notes for Part 2B: important information on the three sections of the exam, available here.
Sample questions: sample SBA and oral questions for the exams have been provided with answers on the RCR website, here for Part A and here for Part B.
Candidate reference sheet: a reference list of abbreviations and normal ranges for use during Part 2A, found here.
Examiners’ reports for Part 2B: this is a collection of generic reports written by examiners on the overall performance of candidates and individual questions as a guide for applicants for future sittings. These are available here.
Understand the SBA format and how to approach questions: this document also provides questions that have been used previously in the Final FRCR (Part A) Examination. You can find this here.
TNM Staging guidance - this document explains the knowledge required to answer questions related to this topic, available here.
Demonstration films: demonstrations of both parts of FRCR Part 2, providing insight into both elements of the exam and what candidates can expect on the day. These are on the RCR website here.
Scoring system for Part 2B: key information on how each part of the exam is marked, found here.
For a detailed guide to the best guidance preparation and courses for the exams, see our blog here.
Sources
https://www.rcr.ac.uk/clinical-radiology/examinations/frcr-part-2a-radiology-cr2a
https://www.rcr.ac.uk/sites/default/files/cr2a_purpose_of_assessment_statement_jan_22.pdf
https://www.rcr.ac.uk/clinical-radiology/examinations/frcr-part-2b-radiology-cr2b
https://www.rcr.ac.uk/sites/default/files/cr2b_purpose_of_assessment_statement.pdf
https://www.rcr.ac.uk/sites/default/files/cr2a_guidance_notes._jan_22.pdf
https://www.rcr.ac.uk/sites/default/files/docs/radiology/pdf/CR2B_scoring_system.pdf
https://www.rcr.ac.uk/clinical-radiology/exams/5faf80dd-7d45-e911-a977-002248072781/dates-fees
https://www.rcr.ac.uk/clinical-radiology/exams/a91e7f01-7e45-e911-a977-002248072781/dates-fees
I’ve passed the FRCR exams! What’s next?
Firstly, congratulations – attaining full FRCR is a massive achievement!
With all parts of the FRCR complete, you have completed the biggest component of the requirements for GMC registration. Once you have completed the English language component, you will be eligible for full GMC registration with a license to practice in the UK.
Don’t hesitate to get in touch with our team to learn more about the opportunities available to you once you’ve passed FRCR.
For the latest news and updates on all things radiology, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.