Search IMG Library
YOUR SPECIALISM- See all
- Gastroenterology
- Microbiology
- Urology
- Rheumatology
- Stroke Medicine
- Ophthalmology
- Oncology
- Neurology
- Histopathology
- Haematology
- ENT Surgery
- Acute Medicine
- Anaesthetics
- Respiratory
- Dermatology
- Geriatrics
- Radiology
- Surgery
- Paediatrics
- Psychiatry
- Emergency Medicine
- Critical Care & ICU
- General Medicine
276 blogs found

MRCP (UK) PACES - a guide for overseas medicine doctors
PACES is the final exam in the MRCP UK examination series.
Attaining full MRCP UK will facilitate registration with the GMC for overseas doctors, allowing you to secure a job in one of the many medical specialties in the NHS, depending on your experience and specialisation. In this article we will consider the following:
What is PACES?
Am I eligible to sit MRCP PACES?
What is the content and format?
How is PACES marked?
As an overseas candidate where can I take the exam?
When should I take PACES?
How can I prepare for the exam?
Passed? What next?
What is PACES?
The Practical Assessment of Clinical Examination Skills (PACES) is designed to test the clinical knowledge and skills of trainee doctors who hope to enter higher specialist training (ST3). The exam sets rigorous standards to ensures trainees are competent across a wide range of skills and are ready to provide high-quality care to patients.
Am I eligible to sit MRCP PACES?
You must have passed the Part 1 written examination within the last seven years before taking PACES. The Royal College strongly advises trainees to apply after competing two years practical experience and Part 2 of the examination.
What is the content and format?
PACES is based on a format that is similar to OSCEs, a practical assessment in a clinical setting. There are five clinical stations with either patients with a given condition, or trained stand-ins (surrogates).
The exam is sat over a half-day and assesses seven core skills over five stations. IMGs can expect eight patient encounters assessed independently by a total of ten examiners (two at each station).
The seven core skills:
Physical examination – demonstrate correct, thorough, systematic, appropriate and professional technique of physical examination.
Identify physical signs – identifying physical signs correctly.
Clinical communication – elicit a clinical history relevant to the patient’s complaints, in a systematic, thorough and professional manner.
Differential Diagnosis – create a sensible, clinically assessed differential diagnosis for a patient.
Clinical Judgment – select an appropriate management plan for a patient or clinical situation. Select appropriate investigations or treatments for a patient that the candidate has clinically assessed.
Managing patients concerns – seeks, detect, acknowledge and address patients or relatives concerns, confirming their understanding and demonstrate empathy.
Maintain patient welfare – treat a patient or relative respectfully and sensitively in a manner that ensures their comfort, safety and dignity.
The PACES Carousel:
The Carousel consists of five stations, each assessed by two independent examiners. Candidates start at any of the five stations, moving round the carousel at 20-minute intervals, until completed. A five-minute period between each station is given.
Candidates are marked on clinical skills at each encounter in the examination. An encounter is when a candidate has an interaction with a patient or a surrogate. Stations 2 and 4 involve one encounter, whereas stations 1, 3 and 5 have two encounters.
How is PACES marked?
PACES is marked on seven skills, A-G, these are:
Skill A: Physical examination (stations 1, 3 and 5)
Skill B: Identifying physical signs (stations 1, 3 and 5)
Skill C: Clinical communication (stations 2, 4 and 5)
Skill D: Differential diagnosis (stations 1, 2, 3 and 5)
Skill E: Clinical judgement (all stations)
Skill F: Managing patients’ concerns (all stations)
Skill G: Maintaining patient welfare (all stations)
Skill B, identifying physical signs, is often considered the most challenging skill to pass.
As an overseas candidate, where and when can I take the exam?
It is a little more complicated than Part 1 or 2 exams and exam slots are often in short supply. Whilst the Royal College is working hard to increase the number of spaces, it is not always possible to offer a place to all applicants.
Priority is given to those candidates who are near the end of their stage 2 eligibility period. A full list of examination dates can be found here, please note these are subject to change.
Examination centres are subject to change, so for up-to-date information, please see the Royal College website here.
The examination is run at clinical centres across the UK (England, Scotland, Wales and Northern Ireland); these vary from diet to diet.
When should I take PACES?
Royal College performance data provides some food for thought when considering when to apply for PACES. The data suggests:
Wait at least 36 months after graduation before applying.
Those taking the exam before this period were less likely to pass.
24-36 months post-graduation – 50% pass rate
36-48 months after graduation – 77%
Candidates that had already passed part 1 & 2 written examinations were significantly more likely to pass PACES at first attempt.
How can I prepare for the exam?
With lots of resources available online, we have discussed with IMGs the best place to start looking for materials relating to the exams. Most IMGs recommended starting with the Royal College, who have created useful resources to help you to prepare for the exams. See below:
Curriculum: Applicants are tested on a range of common and important disorders in General Medicine as set out in the Joint Royal Colleges Specialty Training Curriculum for Core Medical Training.
We recommend getting to know the curriculum as early as possible, using it as a road map for your study plan.
It is recommended that to give yourself the best chance, you gain clinical experience involving care of emergency patients, adults and children.We advise you to regularly invite senior colleagues to observe and provide feedback on your clinical assessments, so you will be comfortable with the PACES format and give you confidence in approaching and examining patients with examiners present.
PACES station 4 examiner guidance examples: This useful guide contains examples of the types of statements found in the examiner guidance section of station 4 scenarios.
This will help you to understand what the examiner is looking for.
PACES sample scenarios: These will provide you with the most accurate and relevant scenarios to prepare you for the real thing. Sample scenarios cover Station 2, 4 & 5 (‘history taking’, ‘communication skills and ethics’ and ‘clinical consultations’ respectively.
Most of these have been previously used in a recent exam, but please note that during the exam you will only receive the section marked ‘information for the candidate’.
Videos on what to expect on the day: These helpful videos will give you a true reflection of what to expect on the day of the exam, easing some of the pressure and ensuring you can focus on the task at hand.
PACES candidate video: Whilst there are lots of useful videos online that are easy to find, the PACES candidate video contains important information about the exam, and practical examples of how the exam will run.
Candidate guide notes: these guidenotes created by the Royal College help IMGs to understand what to expect on the day, from your arrival to the completion of the test.
It can also be useful to understand how IMGs have failed the exam in the past, as this will give you the best chance to pass first time. The ‘how I failed PACES’ guide provides tips to help you to identify where you might be going wrong, along with practical advice to help you to improve.
For a useful overview of how to prepare for exams, including advice on study groups, online community support, best use of online resources & Royal College materials and courses - take a look at our blogs on exam tips and preparation.
Passed? What next?
First of all, congratulations! After you have passed all parts of MRCP (UK) you can apply for a full registration with a license to practice. Once the GMC have approved your application, you can work as a doctor in the UK.
IMG Jobs
Specialise in gastroenterology, respiratory, neurology, dermatology, geriatrics or any other areas within specialist medicine? Search and find live specialist medicine NHS doctor jobs in the UK.
General & Acute medicine? Search for live vacancies here.
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Get in touch using the buttons above (and below) to discuss specialist medicine job opportunities in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.
Follow us on social media for news and updates on GMC registration, the Royal College and NHS through the links below:
UKMLA – Transitioning from PLAB: a guide for IMGs
The UKMLA or MLA (Medical Licensing Assessment) is a new assessment being introduced by the GMC to replace PLAB (Professional and Linguistic Assessments Board) for international medical graduates (IMGs) and UK medical students.
The UKMLA will be the new standard test of the core knowledge, skills and behaviours needed to practise safely in the UK.
In this blog we will be taking a closer look at the assessment and the transition from PLAB, focusing on some key questions:
Why is the MLA being introduced?
Who will need to take the UKMLA?
What is the timeline for the transition?
How will the UKMLA be structured?
Skip ahead to the relevant section if you know what you’re looking for.
Introducing the UKMLA
Currently, PLAB is the assessment used to ensure doctors who qualified abroad have the right knowledge and skills to practise medicine in the UK. Once an IMG has completed both parts of PLAB, they are eligible for full GMC registration.
For UK trainees however, full registration is gained on moving to the second year of the Foundation Programme (F2/ FY2) in an approved training programme.
There is therefore no standard used for both UK medical graduates and international doctors, so the GMC has created the MLA with the stated aim of setting a common threshold for safe practice in the UK, regardless of where a doctor was educated or trained.
UKMLA Candidates
From 2024, all IMGs who would have sat the PLAB test will take the MLA if they’re applying for registration with a licence to practise in the UK. This means that if you are an overseas doctor taking another route to GMC registration, this is still available to you if you are eligible.
UK medical students graduating in the academic year 2024-25 will also need to pass the MLA as part of their medical school degree, before they can join the medical register.
You can find more information about your possible routes to the UK as an international doctor in our detailed guide here.
Transitioning from PLAB to MLA
Until 2024, IMGs will still be able to apply for PLAB in order to gain GMC registration. As overseas doctors wanting to come to the UK through this route will be in different stages of the process, the GMC has laid out the following guidelines which will be in place during the transition to the UKMLA:
I have passed both parts of PLAB
I have passed PLAB 1, but not yet attempted PLAB 2
I have attempted PLAB 1, but not yet passed it
I have passed PLAB 1 and attempted PLAB 2, but not yet passed it
Passed both parts of PLAB
There will be no changes here: you will still have up to two years from the date that you passed PLAB to apply for full GMC registration with a licence to practise.
Passed PLAB 1, but not attempted PLAB 2
As long as you passed PLAB 1 within the past two years, you won't need to take the AKT. However, instead of PLAB 2, you will take the CPSA.
Once you pass the CPSA, you'll be able to apply for full registration with a licence to practise (this must be within two years of passing the CPSA).
Attempted PLAB 1, but not passed it
You will sit the AKT.
There will be a maximum number of attempts and any previous attempts at PLAB 1 will count towards this maximum number. The GMC is currently still finalising that maximum number.
After passing the AKT, you will need to take the CPSA within two years.
Passed PLAB 1 and attempted PLAB 2, but not passed
As long as you passed PLAB 1 within the past two years, you won't need to take the AKT.
Instead of PLAB 2, you will take the CPSA.
There will be a maximum number of attempts and any previous attempts at PLAB 2 will count towards this maximum number. The GMC is currently still finalising that maximum number.
Once you pass the CPSA, you'll be able to apply for full registration with a licence to practise (this must be within two years of passing the CPSA).
Structure & Format of the UKMLA
The UKMLA will be composed of two parts: the applied knowledge test (AKT) and the clinical and professional skills assessment (CPSA). Both components will assess a range of things, all of which are outlined in the MLA learning outcomes. The main purpose of the MLA is to assess the knowledge and competencies related to safe medical practice in the UK.
1. The applied knowledge test (AKT)
This is planned to be an on-screen exam, with multiple choice questions. It will test your ability to apply medical knowledge to different scenarios. The AKT will be similar to the current PLAB 1 exam.
The AKT for overseas doctors will be set by the GMC, whereas for UK medical students, the exam will be run by medical schools. Information from the UK exams will be used to ensure that the assessment is comparable and consistent, where appropriate.
The test is expected to be held four times a year for international candidates, at a number of locations worldwide.
You will need to pass the AKT before you can take the CPSA.
2. The clinical and professional skills assessment (CPSA)
The CPSA for international doctors will be held at the GMC’s clinical assessment centre in Manchester. The CPSA will be similar to the current PLAB 2 exam.
For UK medical students, the CPSA will be set and run by their medical school. Each UK medical school calls the CPSA something different e.g. an Objective Structured Clinical Examination (OSCE), however the GMC will set requirements that all CPSAs must meet.
Exam Structure
The MLA content map tells you more about the topics and areas that your AKT and CPSA assessments could cover.
The MLA has three overarching themes: readiness for safe practice, managing uncertainty, and delivering person-centred care; and six sections, called domains.
Areas of clinical practice, such as mental health and surgery
Areas of professional knowledge, such as biomedical sciences and medical ethics and law
Clinical and professional capabilities, such as assessing and managing risk and safeguarding vulnerable patients
Practical skills and procedures, as set out in the list of practical skills and procedures that supplements the GMC’s Outcomes for graduates (2018)
Patient presentations, which relates to signs, symptoms, investigation results and other relevant patient-related issues typically seen by doctors in a first appointment within the UK Foundation Programme e.g. a chronic rash or breast lump
Conditions, which are pathophysiological diseases or clinical diagnoses typically seen by doctors in a first appointment within the UK Foundation Programme e.g. asthma and eating disorders
In the future, sample questions will be provided by the GMC for the AKT so that you can get a better feel for the test.
Other Key Information
Cost
Similarly to PLAB, you will have to pay a fee to sit the UKMLA as an IMG. The fees have yet to be set by the GMC, but will be published once determined.
EEA Graduates
Decisions about whether EEA graduates will need to sit the MLA from 2024 will be informed by government-led agreements and trade deals. The GMC will provide an update on this situation once there is more information about future arrangements.
English Language Requirements
The MLA won't change the GMC’s English language requirements for registration. You must still prove that you have the necessary knowledge of English to practise safely in the UK.
Sources
https://www.gmc-uk.org/education/medical-licensing-assessment
https://www.gmc-uk.org/education/medical-licensing-assessment/uk-students-guide-to-the-mla
The introduction of the UKMLA is a significant change to one of the most popular routes taken by IMGs wanting to work in the NHS. Despite the change, there are always several options available to overseas doctors wanting to relocate to the UK. Feel free to get in touch with our team to discuss your options.
Read more useful articles on exams, NHS jobs and salaries in our IMG Resources library.

What Brexit means for you
On 23rd June 2016, the UK voted to leave the European Union (EU).
The exact terms of the process by which the UK will depart the EU are still unclear and may remain so for some time due to the urgent attention the COVID-19 coronavirus requires. As such, IMG Connect will continue to review our guidance for EU Nationals relocating to the UK, but for now there are some steps that you can take to explore your rights as an EU citizen.
At IMG Connect we support every single one of our international friends and doctors, and we know that the NHS is enhanced by the contribution of doctors from every country in the world. The contribution of EEA doctors to the NHS is hugely significant across all areas of medical practice.
What does Brexit mean for you so far…
The status of EEA doctors already registered with the UK is guaranteed. But it is unclear whether current GMC registration arrangements for EEA doctors*, which are based on the principle of mutual recognition of doctors’ qualifications and enables the GMC to grant registration very quickly, will continue after the UK leaves the EU in 2019.
The UK government has reached an agreement with the EU that will protect the rights of EU citizens and their family members living in the UK. It has also reached an agreement with Norway, Iceland and Liechtenstein, and a separate agreement with Switzerland.
These agreements mean that most citizens from the EU, Norway, Iceland, Liechtenstein and Switzerland will need to apply to stay in the UK.
*The EEA includes EU countries and also Iceland, Liechtenstein and Norway.
EU Settlement Scheme:
If you’re an EU, EEA or Swiss citizen, you and your family can apply to the EU Settlement Scheme to continue living in the UK after 30 June 2021. If your application is successful, you’ll receive either settled or pre-settled status. You may be able to stay in the UK without applying - for example, if you’re an Irish citizen or have indefinite leave to remain.
The EU Settlement Scheme is open and free to apply. You can apply now if you meet the criteria. The deadline for applying is 30 June 2021. Use the Government online toolkit to find out what you need to do and when. You will need to be living in the UK before it leaves the EU to apply. The deadline for applying will be 31 December 2020.
What else can I do?
Of course, there remains uncertainty over the impact that Brexit will have on the laws regarding immigration in the United Kingdom.
So, we must stress that the information above is for general information purposes only and it may not always be up-to-date. We will do our upmost to keep informed and be in a position to support our EEA colleagues, for whom who we have the highest regard.
We encourage all doctors to join our community, and show their support, field any concerns, or share and answer questions to stay connected. You can always get in touch with us at IMG Connect by requesting a call back with anything you need help with - we are here to support you individually and collectively.
How will the coronavirus affect the UK leaving the EU?
It is very hard to say how exactly how the COVID-19 outbreak will affect Brexit, if at all. Certainly the pandemic has caused the government to divert all attention on keeping the pandemic contained and matters relating to Brexit and immigration status are not being discussed with the same urgency they were previously. Whilst we endeavor to stay up to date with how these things affect EU doctors and their immigration status, we strongly advise that you stay in touch and up to date with the Government website and updates here.
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Get in touch using the buttons above (and below) to discuss doctor job opportunities in the NHS, including discussions regarding a typical doctor salary in the UK and the most suitable hospital locations for you.
For regular news and updates, follow IMG Connect on social media using the links below:

Career Pathway for a UK Doctor in Training
The NHS offers extensive training schemes and career development for all of its doctors, and such programmes are recognised as a gold standard across the medical world.
Training in the NHS is always in keeping with advances in medical sciences and the progressive landscape of the medical profession, including the more complex ailments of a growing and ageing population. The NHS frequently updates and develops its training programmes, making them attractive to UK graduates and doctors, as well as overseas doctors seeking the very best training.
In this article we will cover the following topics:
The NHS Training Pathway
Graduation to Foundation Training
Specialty Training Programmes
Different types of Specialty Training programmes
Completion of Specialty Training Programme
Should I apply for a training or service post?
As an IMG, can I get onto the specialist register?
How do I secure a service post?
Skip ahead to the relevant section if you know what you're looking for.
The NHS Training Pathway
Many IMGs looking to move to the UK (particularly more junior doctors) will be keen to enter into UK Specialty Training at some point, and as such it is important to understand the UK training pathway from start to finish in order to map your NHS career effectively.
Furthermore, greater understanding of the NHS structure and training offered to doctors in the UK will help an IMG to understand at what grade they can likely enter the system and the salary most appropriate for them.
The NHS Training Pathway describes the journey from medical school to completion of specialist training and is the path most commonly followed by UK trainees.
Graduation to Foundation Training
After graduating from a medical school, doctors gain provisional registration with the GMC allowing them to enter the Foundation Programme - a two-year work-based training programme.
Upon completion of the first year (FY1 or F1) doctors will gain full registration with the GMC and can apply for further study and training in a specialised area – known as Core or Specialty Training, depending on the specialty.
Specialty Training Programmes
Completion of the Foundation Programme allows doctors to apply for Specialty Training in an area of medicine or general practice. There are 60 different specialties to choose from.
A doctor entering year one of Specialty Training is known as an ST1 or CT1 doctor.
Specialty Training programmes can take between three and eight years depending on the specialism chosen.
Doctors can pass through the training quicker depending on how fast they achieve their competencies.
Sometimes doctors do not complete the training pathways in the indicated time for a variety of reasons and it can take between 1 - 4 years longer than indicated in the curricula.
Types of Specialty Training Programmes
There are two different structures for Specialty Training programmes, and these vary between specialties.
Run-through Training Programmes
For these training programmes, you only have to apply once at the beginning of the programme. This is because you are recruited for the full duration of Specialty Training.
These training programme can last from approximately three years for general practice, to five or seven for other specialties such as histopathology.
Uncoupled Specialty Training Programmes
These programmes are split into Core Training and Higher Specialty Training.
Core Training lasts for either two or three years and once complete, allows you to apply for Higher Specialty Training, which can take from three to five years.
Overall, Specialty Training programmes can take anywhere from 5 – 8 years in their entirety, depending on your medical specialty, for example 6 years for psychiatry.
Doctors are known as ST1-3 or CT1-3 during their Core Training and ST4+ level during Higher Specialty Training programmes.
Higher Specialty Training programmes are very competitive, and completion of a UK Core Training programme does not guarantee a Higher Specialty Training post.
Completion of Specialty Training Programme
Upon successful completion of either a run-through or coupled training programme, doctors are awarded a Certificate of Completion of Training (CCT).
At this point doctors are able to make an application for Specialist Registration (or GP Registration) and are able to take up permanent consultant posts.
Training Positions vs Service Posts
As above, competition for places on training programmes within the NHS is very high. As such, we advise that IMGs who are interested in entering core or specialty training in the NHS first obtain a service post for 1 – 2 years.
Following this contract, you can apply for a training post, for which you will be given priority. Not only will this approach give you the best chance of securing excellent training and career progression opportunities in the NHS, it will also give you the chance to settle in to the UK and the NHS system, and help you understand the training post that will suit you the most.
Service posts also offer very competitive rates, so whilst you are getting to know the NHS and settling into life in the UK, you can also ensure that you are financially rewarded.
Specialist Registration for IMGs
IMGs that enter the UK training programmes later on and have not completed the full programme can still get on the specialist register via the CESR-CP route (Certificate of Eligibility for Specialist Registration via a Combined Programme)
Check to see if you're eligible for CESR-CP via the GMC website or read through our detailed blog through our IMG Resources library.
Secure a Trust Doctor Post (with the view to securing a training post at a later date)
You can apply for Trust Doctor or Service Role online via the NHS Jobs website.
However, working with IMG Connect can offer more jobs than are available online with the added benefit of an IMG Consultant speaking directly with services on your behalf to expedite the process and negotiate the best doctor salary for you.
Getting started
Read more useful articles on finding an NHS trust doctor job, training pathways, doctor salaries in the UK, relocation and much more!
Don’t hesitate to get in touch with our team to learn more about the opportunities available to you once as an IMG new to the UK.
For the latest news and updates, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation:

Preparing for Royal College Exams - a guide for IMGs
It can be quite difficult to juggle the demands of everyday life such as clinical work and family commitments with preparing for the Royal College exams. This is particularly the case for IMGs who may be completing these exams alongside training and exams in their own country.
In this blog, we will share some great tips we’ve recommended by overseas doctors we’ve worked through after passing their UK postgraduate exams.
1. Plan ahead
It is important to set feasible targets when taking on postgraduate study, so carefully consider your personal circumstances and set a goal for when you are going to take the examinations.
You should try to avoid any major life events at the time of the events e.g. weddings, moving house etc.
2. Use the curriculum
The blueprint for the Royal College exams is the curriculum used in the training programme for each specialty, and we always recommend this as the best place to start.
UK trainees will be familiar with this as part of their training and continued assessment, so international doctors should familiarise themselves with the curriculum and any syllabus as soon as possible.
Curriculum for MRCP, MRCEM, MRCPsych, FRCPath, FRCR, FRCR (Oncology), MRCPCH, MRCOG and MRCS.
3. Familiarise yourself with the exam structure and format
It is important to know exactly what you can expect from the exam, such as whether the exam will be remote or what different topics the exam comprises. This will help you to create a structures and comprehensive plan as you begin your revision.
You can find a detailed overview of the Royal College exams in our IMG Resources library.
4. Create your own study programme
Create a manageable and realistic study plan based on the time you have until the exam. Be sure to build in suitable breaks and time off to allow you to proceed with your study at a steady pace.
Think about your personal learning style and use this to plan effective revision.
5. Find the best study materials to suit your needs
There are many online resources available from commercial courses to question banks and notes, which daunting for IMGs. We recommend looking at what seems to be most popular among other IMGs, such as the Bromley courses for MRCEM, SPMM mock exams and notes for MRCPsych or Pathology Online Hub courses for FRCPath Histopathology.
Where there is a large cost associated with the resources, perhaps you can see if any colleagues would like to split the expense or has copies they can lend to you.
Also, don’t be afraid to tailor these resources to suit your study needs – make notes or mind maps to aid learning and revision.
6. Build on your existing knowledge base and experience
You will likely be familiar with many of the concepts in the exam from your own clinical experience – take advantage of this is your study. Use your knowledge and experience from your own country and training as the foundation for your revision.
7. Try to maintain a balance between work and personal life
As much as possible, try not to overload yourself with study and make time for study breaks where you can focus on your personal life and having some downtime.
8. Practise, practise, practise...in the expected exam format
Crucially, you must practice exam-style questions as much as possible within the time you have. This not only helps you to understand where you have any deficits in your knowledge, but also shows you what to expect in the types of questions asked and how they may be phrased. It is also important to reinforce memory by revising and by practising recall.
For clinical exams such as an OSCE or CASC, you should practise these with others and observe others practising too in order to obtain feedback.
9. Join a community of like-minded doctors
Belonging to a study group may help you reduce your workload of finding information and enable you to share experience and provide support to each other. Study groups also aid reflection on progress.
IMG Connect host two fantastic Facebook groups for overseas psychiatry and pathology doctors where we share guidance, resources and study courses. You can join our communities here: IMG Psychiatrists and IMG Histopathologists.
We hope you find these tips helpful and wish you the best of luck with your exams. Don't forget to share your successes with us on social media using the hashtag #imgstories
To receive the latest news and updates on the Royal Colleges, GMC registration and the NHS, follow us on social media and join the conversation.
Get in touch
Have you completed the Royal College exams? Get in touch with one of our dedicated recruitment specialists to discuss your next steps towards GMC registration, finding work in the NHS and relocating to the UK.
CESR - a comprehensive guide for medical oncologists
Doctors from any country can apply for Specialist Registration in the UK, provided they meet certain eligibility criteria, though there are different routes available based on the doctor’s training and qualifications.
In this blog we’ll be exploring Specialist Registration in medical oncology for overseas medical oncologists more closely. We’ll look at all aspects of Specialist Registration, focusing more closely on the Certificate of Eligibility for Specialist Registration (CESR), including the application process, costs, and eligibility criteria, along with some other topics, summarised in the headings below:
What is Specialist Registration?
What route is best for me as an overseas oncologist?
Do I have to complete CESR before I can work in the UK?
Do I need MRCP (UK) for Specialist Registration?
What is the CESR equivalence process?
What evidence do I need to submit for a CESR in medical oncology?
How much does CESR cost?
How long is the CESR application process?
#IMG Tips
How do I get started?
Skip ahead to the relevant section if you know what you’re looking for.
Specialist Registration
Holding Specialist Registration in any CCT specialty means that you can be appointed to a substantive (or permanent) consultant position in the NHS. All medical oncologists who wish to take permanent consultant roles in the UK must show evidence of skills, knowledge, and experience equivalent to a CCT in order to apply for Specialist Registration.
For oncologists, attaining specialist registration will mean you are qualified to practice independently as a medical oncology consultant in the NHS.
Specialist Registration is additional to full registration with the GMC and is therefore not required to practice as a medical oncologist in the UK.
Routes to Specialist Registration
There are three types of certificates issued by the GMC for Specialist Registration, and the type of certificate you receive depends on the training route you followed.
CCT for UK-trained Oncologists
For doctors who have completed a GMC-approved training programme, an application must be made to the GMC for a CCT in their specialty within 12 months of their completion date in order to qualify. After this point, they will be required to use the CESR route to apply directly to the GMC if they wish to attain Specialist Registration.
CCT for EEA-trained Oncologists
Doctors who have trained outside the UK or Switzerland, but within an EEA country, will be awarded CCT (Certificate of Completion of Training) after a successful specialist registration application. Specialist Certifications from across the EU are deemed as equivalent by the GMC, and therefore a straightforward application can be made. You can read more about this in the Specialist Registration section under your country on the GMC website here.
CESR-CP for Oncologists who have complete part of a GMC-approved training programme
CESR(CP) is a simplified route to Specialist Registration for doctors who joined their specialty training programme after ST1, and therefore do not meet the requirement of 4 years duration in GMC-approved training on completion, as they began their training overseas and completed it in the UK.
CESR for Overseas Oncologists
For overseas doctors who have completed their full training outside a GMC-approved training programme, CESR is the route they will usually take towards attaining Specialist Registration. This route does not require further training, rather the submission of an application.
You can read a detailed breakdown of Specialist Registration in the UK in our IMG Resources library.
Medical Oncology Positions in the NHS without CESR
It is important to note that you can apply for senior oncology roles in the NHS, such as a specialty doctor (SAS), specialist grade or a locum consultant without being on the Specialist Register.
Similarly, CESR is not required by overseas doctors before moving to the UK to work in the NHS.
In these senior NHS roles, you will have better pay and responsibilities that are more appropriate to your level of experience compared to a trainee. Within these positions, you can collect evidence of your competences, particularly those specific to the UK medical oncology curriculum.
These positions also facilitate a faster route to the UK than the CESR route, which can take a substantial amount of time.
Get in touch with us to find out more about senior positions in the NHS with CESR support.
MRCP (UK) for Specialist Registration
Whilst it is always beneficial to complete MRCP (UK), particularly for doctors who have trained outside of the UK or an EEA country, overseas doctors looking to join the Specialist Register do not need to have completed the Royal College postgraduate exams.
The standard test of knowledge in the Medical Oncology curriculum are the MRCP (UK) exams, so passing these exams confirms the attainment of the competencies of the core curriculum.
MRCP (UK) is only a requirement for doctors looking to attain Specialist Registration via the CCT route.
The structure of the programme is an indicative two years in Core Medical Training or Acute Care Common Stem (ACCS), followed by an indicative four years of training in Medical Oncology. Therefore, applicants need to demonstrate the appropriate level of acute medicine expertise as well as competencies in medical oncology.
You can read more about the evidence required in the specialty specific guidance here.
CESR Equivalence Process
Equivalence describes the process of assessing an overseas applicant’s training and experience against the current medical oncology training programme requirements, in order to be awarded CESR.
The equivalence process involves submitting a written body of evidence to the GMC, consisting of:
training and/or competence
skills and knowledge
The Royal College of Physicians will assess each application against the relevant curriculum before providing a recommendation to the GMC, who will then make a decision.
Please note that Equivalence procedures are the responsibility of the GMC. Applications are made through their Certification Department and initial enquiries should be directed there.
Evidence Requirements for CESR in Medical Oncology
Skills & Experience: The evidence provided for a CESR application in oncology must cover the knowledge, skills, and qualifications to demonstrate the required competencies in all areas of the Medical Oncology Curriculum. If evidence is missing from any area of the curriculum, the application will fail.
Primary Evidence: To demonstrate that you can do what is required by the curriculum, you need to submit primary evidence of your medical practice which shows how you work on a day-to-day basis: letters, reports, assessments etc. References, retrospective case summaries, and reflective notes can all be used in a CESR application, but by themselves they are not sufficient.
Audit and Governance: You are required to submit evidence of your active leadership in audit, including evidence that you have completed at least one audit cycle
Currency of evidence: Your evaluators will be looking for evidence of current competency, generally defined as within the last five years. If you have completed training before this point, it is crucial that you provide evidence of maintaining competency across the whole area of the curriculum.
The GMC asks that only evidence that is strictly relevant is sent as it will help them to process the application quicker. The guidance on compiling your evidence will help you to decide what is relevant and what is not – you can find this on the GMC website here.
As a general guide, the GMC usually expects to see about 800 - 1000 pages of evidence, divided into four different domains, reflecting those of Good Medical Practice. The GMC recommends that you apportion the evidence provided as shown below:
Domain 1 – Knowledge, skills, and performance
Domain 2 – Safety and quality
Domain 3 – Communication, partnership, and teamwork
Domain 4 – Maintaining trust
Please note, you cannot compensate for evidence lacking in one area by providing more evidence in another area.
The full list of evidence required for each domain can be found on the GMC website here.
CESR Application Cost
All oncologists applying for Specialist Registration must pay a fee. As of 1st April 2022, for CESR, this fee is £1,727. For CESR-CP and CCT, the cost is £452.
How long does it take to complete an application for CESR in Medical Oncology?
The GMC estimate that it can take between six and eight months to receive a decision, from the date you submit your CESR application.
As there is a substantial amount of evidence to gather for a CESR application, the process of preparing all the necessary documentation and applying for CESR can take even longer than this, and a typical candidate will usually set out to complete this within 1 – 3 years.
It is worth noting that more senior oncologists, such as consultants, are more likely to have achieved all the competences outlined in the curriculum.
The indicative period of training for a CCT in medical oncology is six years, so it is highly unlikely that you would achieve the competencies required for a CCT in a shorter period of time. Therefore, CESR is not suitable for more junior oncologists.
#IMG Tips
Research/think about the types of evidence you will need and begin to gather your evidence well in advance of making your application.
Gather evidence prospectively – this is much easier than retrospectively trying to pull together the evidence under additional pressures.
Make sure that your evidence is of the highest possible quality and is current – you will be assessed against the most recent curriculum.
Ensure that the evidence you collect demonstrates your competence across the whole of the Medical Oncology curriculum, not just your sub-specialty.
Remember to refer to the most up-to-date Medical Oncology CCT Curriculum and Specialty Specific Guidance for the evidence requirements in your specialty.
Create a CESR ‘to-do list’ with sections under the GMC’s 4 domain headings – organise your evidence directly into these sections to manage your progress.
Do not submit original documents – all your copies, other than qualifications you’re getting authenticated must be accompanied by a proformas signed by the person who is attesting to the validity and accuracy of your evidence (your verifier).
Ask an IMG Connect recruitment specialist about NHS oncology posts with CESR support. These are not always advertised by a Trust, but we can help you find a role which aligns well with your career goals in the NHS.
Join the online community - join the IMG Oncologists Facebook group for access to a community of like-minded MRCP aspirants and dedicated oncology recruiters.
In this group you will find tailored resources for oncology IMGs, including access to our MRCP crash courses, completely free to all doctors.
You can access our IMG Oncologists community here.
Sources
https://www.jrcptb.org.uk/certificate-eligibility-specialist-registration
https://www.gmc-uk.org/registration-and-licensing/join-the-register/registration-applications/specialist-application-guides/specialist-registration-cesr-or-cegpr
https://www.gmc-uk.org/-/media/documents/sat---ssg---medical-oncology---dc2310_pdf-48455474.pdf
Getting started
Many oncology IMGs likely haven’t completed a UK-approved training programme, but you could be eligible for Specialist Registration with the GMC via the CESR route. Take a look at our guide to CESR applications for medical oncology for more information on how to apply and what to expect.
If you have any further questions about Specialist Registration, your route to the UK, or would like guidance in finding NHS posts which offer CESR support, please get in touch with us here.
Follow us on social media through the links below for regular news and updates on the Royal Colleges, relocating to the UK and working in the NHS:

My Experience of MRCEM Primary - Dr Behzad Rashid
Are you an overseas emergency medicine doctor taking the postgraduate route to GMC registration through the MRCEM exams? Are you interested in sitting the exams in the future?
As part of IMG Stories, we introduce to you Dr Behzad Rashid, an emergency medicine doctor who has recently sat and passed the MRCEM Primary exam. Dr Rashid will be sharing with you his experiences of the first of the Royal College of Emergency Medicine exams, taking you through his preparation, experience of sitting the exam and sharing some hot tips for international MRCEM aspirants.
Tell us about yourself... what should the IMG Community know about Behzad Rashid?
I am a Resident Emergency Medicine Physician, currently working in Pakistan and have worked in A&E since completing my internship. I started off as a medical officer, and then began an A&E residency programme in my country. I would say a combination of hard work and fate are the reason why I am where I am today.
What motivated you to sit the MRCEM exams?
I had booked a space on the PLAB 1 exam, however, due to COVID, it was unfortunately cancelled (three times in fact). By the third time, I’d had enough. I decided to progress my career in Pakistan because I felt I wasn’t getting anywhere with the exam bookings, and everything was very uncertain at that time.
Even though time felt like it had stopped, it was actually flying by. I therefore decided to sit the residency exam in Pakistan. I worked in A&E at the time and had heard about the MRCEM exams from my colleagues. Due to the lockdown, they had just announced that the exam could now be taken online, even within the comfort of your own home. I was ready to go all in and grind my way through both exams, so I studied and succeeded in clearing both PLAB 1 and MRCEM Primary.
At what point in your career and training did you sit the MRCEM Primary exam?
There wasn’t anything in particular that made me realise that I was ready to sit this exam, besides the fact that COVID had been ruining my plans. I was going through a difficult time, and A&E was something I dearly wanted to pursue. I saw an opportunity, and I took it.
Applications can be frustrating… how did you find the application process for the exam?
The whole process took me about 30-45 minutes to complete. The details of application and exam are available on the website, and whilst a bit tedious, it is a straightforward process. Based on the RCEM’s eligibility criteria for the first exam, you only need to have graduated with an approved medical degree in order to sit the exam.
Since I was planning to sit the exam in my own country, I was provided with some options for exam centres. There were multiple private exam centres nearby, and I did not want to sit the exam at home and risk the internet issues others had experienced. I booked my exam for 8 am, because that's when I function best, and I would recommend that everyone books whatever time of day you think you would perform best.
How far in advance did you start preparing for the MRCEM Primary?
I booked the exam 4 months in advance (around the end of October, with the exam in Dec). Everyone has their own method of studying, and for some, this may not be enough time, so whatever schedule has worked for you in the past - stick to it. In my opinion this exam requires about 3-4 months of studying if you are unemployed or have any daily commitments, and about 5-6 months if you are working or have a very busy schedule.
Often IMGs are a bit at a loss to get support... did you benefit from speaking to senior colleagues or peers about the exam? Did you study with other candidates?
I was in touch with a few individuals who had already sat the exam. They guided me through the application process and resources I could use to prepare. They were also the ones who entertained my idea in preparing for both exams at once, and they believed that I could succeed in both.
You don’t need a lot of friends, just the right ones who will push and support you in your journey.
You were preparing for PLAB at the same time as the Royal College exams...how do you feel studying for PLAB 1 compares to your experience of MRCEM Primary?
PLAB 1 and MRCEM Primary are completely different exams.
PLAB 1 focuses on the application of medical knowledge in common day-to-day scenarios that a doctor would encounter in the UK. MRCEM Primary is more of a theoretical assessment of the basics i.e. anatomy and physiology of emergency related scenarios. This became even more apparent after I’d gone over the curriculum provided by the GMC and RCEM, which is honestly the best part of the exams. I would not say that one is easier than the other – they assess different things.
I focused on the blueprint/curriculum for each exam and made sure to get in as many MCQs as possible. That gave me a better overview of what I would actually be tested on.
Emergency medicine doctors are notoriously busy...in the months leading up to the exam, how much time did you spend a week on preparation?
In my case, I had to appear for the MRCEM Primary first, and then a week later for the Pakistan Residency (FCPS I) exam. Since work was extremely hectic, and I felt that I was not able to set aside much time to prepare for both, I quit my job to study for the exams and managed my time throughout the day to study and prepare for both (around 12 hours each day).
It goes without saying that any goal without a plan is just a wish. I divided my day into 2 halves where I would wake up at 5am, and study till 12pm, take a break (which included sleeping, eating or working out), then start off again at 5pm and go at it till 10pm. The first half would be MCQS and making Anki flash cards, second half would be to review the cards I had pending for that day. I would throw in a mock exam every week to see where I stood at that point, correct my mistakes and make cards on those as well. I stuck to this routine for 3 months and by the end of the 3 months, I had a deck of about 2000 Anki flash cards, divided into two groups for the 2 exams, and that is all I would review because I was confident that is all they would test me on.
How did you manage to juggle other commitments whilst studying for the exam (without panicking)?
During COVID, I was pretty much stranded by myself in Pakistan. My family lived in a different country, and I had limited interactions with the family I did have around me. This bizarre period of isolation and confusion gave me ample time to prepare for my exams. Being alone did get frustrating at times, and anxiety would creep up on me, but the hunger to clear my exams and progress my career gave me tunnel vision and cancelled out all the other noise.
The preparation for 2 examinations was an enlightening and humbling experience. My goal is to reach out to students and help them understand what works best for them. I’d be more than happy to provide students with any resources (Including my Anki flash cards) they need. However, there isn’t a cookie cutter plan that will suit everyone - I did what was best for me in my circumstances, and you must do the same.
What resources did you use to prepare and practice for the MRCEM Primary exam?
I used the curriculum provided by the MRCEM on their website which you will find here.
Along with that I was using the MRCEM Success question bank, which I have to say is an excellent resource. The actual exam was very close to the MCQs provided, which is why I would highly recommend it.
I am also an avid user of Anki. It has helped me ace exams in med school, the MRCEM primary, FCPS I and even the PLAB 1. I have never made any notes from any textbooks, and I honestly think hardcovers will eventually become obsolete. I would highly recommend making your own cards since that allows you to work at your own pace and address any weak points. I would love to share my own deck of Anki cards as well, which covers everything provided in the MRCEM curriculum. Feel free to add more to this deck and pay it forward.
Let's face it, exams are not everyone's favourite day out... so on the day of the exam, what did you do to relax?
I woke up early and decided not to go over any cards. I’m the type of exam-taker who enjoys working out and listening to music before an exam. At that point, I know what I know, and that is all I know. So I drank a nice cup of coffee and got some cardio done while listening to music.
What was your experience like on the day?
My exam was around 8:30am, so the drive was about 5 minutes to the exam hall and I got there around 30 minutes before it started. The invigilator was friendly and after leaving my personal belongings in a small locker, they provided a sheet of paper and stationary at the centre. The computer prompted me to start once the invigilator asked me to, and everything after that went smoothly. The invigilators are ready to help you with your queries if you experience any problems during the exam as well.
What was the most challenging part of the exam?
In my honest opinion, I did not come across anything that would throw me off. After going over the curriculum, and having a plan, I just stuck to that plan and followed it till the end.
In hindsight, would you have done anything differently?
I was already taking the most extreme measures by preparing for multiple exams and taking time off work, given everything was shut down during COVID. I have no regrets and cannot think of anything I’d have done differently.
What nuggets of advice would you give to any MRCEM Primary aspirants?
The best thing about the Royal College exams is that they provide a curriculum of what you should know, and they would never ask anything more than that. I would highly recommend you go over that and familiarise yourself with the content you will be tested on. Question banks might provide extra information to give you a different perspective of the subject, however the real exam sticks to its curriculum. If you know what you are required to know, preparation for the exam becomes easier.
What are your plans going forward?
I'm planning on appearing for the PLAB 2 and the MRCEM Intermediate soon. I have already started preparing my Anki deck for the intermediate as well, so wish me luck and stay tuned for that as well.
To learn more about the RCEM exams, see our IMG Resources library.
For news and updates on all things emergency medicine, follow us on social media and join the conversation.

Preparing for PACES - where do I start?
As an overseas doctor where should you start with your PACES exam preparation?
With lots of resources available online, we discussed with successful candidates for them the best place to start looking for exam materials. Whilst there are lots of fantastic courses available for IMGs to help pass their PACES exam first time, most IMGs recommended starting their preparation with free resources from the Royal College of Physicians. Using these will give you strong foundations to further supplement with any further studies or courses which you may decide to invest in.
We have provided the Royal College's official resources below:
Curriculum
PACES station 4 examiner guidance examples
PACES sample scenarios
Videos - what to expect on the day
PACES candidate videos
Candidate guidenotes
PACES marksheets
General Exam Tips & Preparation
Passed? What next?
It is recommended that to give yourself the best chance, you gain clinical experience involving care of emergency patients, adults and children.
We advise you to regularly invite senior colleagues to observe and provide feedback on your clinical assessments, so you will be comfortable with the PACES format and give you confidence in approaching and examining patients with examiners present.
Curriculum:
Applicants are tested on a range of common and important disorders in General Medicine as set out in the Joint Royal Colleges Specialty Training Curriculum for Core Medical Training.
We recommend getting to know the curriculum as early as possible, using it as a road map for your study plan.
PACES station 4 examiner guidance examples:
This useful guide contains examples of the types of statements found in the examiner guidance section of station 4 scenarios. This will help you to understand what the examiner is looking for.
PACES sample scenarios:
These will provide you with the most accurate and relevant scenarios to prepare you for the real thing. Sample scenarios cover Station 2, 4 & 5 (‘history taking’, ‘communication skills and ethics’ and ‘clinical consultations’ respectively.
Most of these have been previously used in a recent exam, but please note that during the exam you will only receive the section marked ‘information for the candidate’.
Videos - what to expect on the day:
These helpful videos will give you a true reflection of what to expect on the day of the exam, easing some of the pressure and ensuring you can focus on the task at hand.
PACES candidate video:
Whilst there are lots of useful videos online that are easy to find, the PACES candidate video contains important information about the exam, and practical examples of how the exam will run.
Candidate guidenotes:
These guidenotes created by the Royal College help IMGs to understand what to expect on the day, from your arrival to the completion of the test.
PACES Marksheets:
To help you understand how PACES is marked here are some examples of full marksheets.
It can also be useful to understand how IMGs have failed the exam in the past, as this will give you the best chance to pass first time. The ‘how I failed PACES’ guide provides tips to help you to identify where you might be going wrong, along with practical advice to help you to improve.
General Exam Tips & Preparation:
For a useful overview of how to prepare for exams, including advice on study groups, online community support, best use of online resources & Royal College materials and courses - take a look at our blogs on exam tips and preparation.
Passed? What next?
First of all, congratulations! After you have passed all parts of MRCP(UK) you can apply for a full registration with a license to practice. Once the GMC have approved your application, you can work as a doctor in the UK.
IMG Jobs
Search and find live NHS doctor jobs in the UK
IMG Resources
Read more useful articles on finding an NHS trust doctor job, pay scales & doctor’s salary in the UK, relocation and much more!
Get in Touch
Don’t hesitate to get in touch using the buttons above (and below) to discuss doctor job options in the NHS, including discussions regarding CESR, a typical doctor salary in the UK and the most suitable NHS jobs & hospital locations for you.
Follow us on social media for news and updates on GMC registration, the Royal College and NHS through the links below:

Final FRCR (Part 2A & 2B) – guidance and resources for IMGs
Overseas radiologists often ask us how to best prepare for the Final FRCR Part 2A and 2B exams. With so much online content geared towards UK trainees, it can be difficult to know what is best suited to you as an international candidate.
Here we have compiled some of the best advice and resources available to help overseas radiologists prepare for their Royal College (RCR) exams. We’ll also address some of the changes to the exam, both the format, administration and availability of the exam for IMGs.
The topics we’ll cover are as follows:
A recap of FRCR CR2A and CR2B
What resources are available for IMGs?
Royal College Resources
Courses
Books
#IMG Tips
Skip ahead to the relevant section if you know what you’re looking for.
An Overview of FRCR CR2A and CR2B
As a quick reminder, Final FRCR refers to the final two exams in the Royal College of Radiologists examination suite for clinical and diagnostic radiologists. The full series - Part 1, Part 2A and 2B – is required by overseas radiologists when applying for GMC registration through the postgraduate route.
FRCR CR2A assesses knowledge of the pathology, imaging techniques, congenital abnormalities and radiological findings that underpin clinical radiology practice.
The FRCR 2A exam consists of 2 papers sat on the same day; each paper containing 120 single-best-answer questions (240 questions in total). Each paper lasts 3 hours.
CR2B is not an exit exam but is a key step in a trainee's progress towards independent reporting. The exam assesses several aspects of the candidate's radiological skills, all of which are considered necessary for safe and effective radiological practise.
Part 2B has 3 separate sections as below:
Rapid reporting - 30 plain radiographs in 35 minutes
Reporting (long cases) - 6 cases in 75 minutes
Oral (viva) - 2 x 30-minute vivas
In total, the exam lasts 2 hours and 50 minutes.
For a full overview of the FRCR exam series, see our blog here.
Preparation & Revision Resources
After discussing with IMGs the best way to approach preparing for the Final FRCR exams, most recommended beginning with the Royal College website and resources, which they have put together to aid in your preparation.
Curriculum: The FRCR exams are based on the Specialty Training Curriculum for Clinical Radiology. As a rule of thumb, your revision should start here to ensure you are focusing on the exact material that will be in your exam. Knowing the curriculum is key and you can find these on the Royal College website here.
Royal College Resources
Instructional video: demonstrations of both parts of FRCR Part 2, providing insight into both elements of the exam and what candidates can expect on the day. These are on the RCR website here.
Guidance notes for Part 2A: a guidance document on key elements of the exam, found here.
Guidance notes for Part 2B: important information on the three sections of the exam, available here.
Sample questions: sample SBA and oral questions for the exams have been provided with answers on the RCR website, here for Part A and here for Part B.
Candidate reference sheet: a reference list of abbreviations and normal ranges for use during Part 2A, found here.
Examiners’ reports for Part 2B: this is a collection of generic reports written by examiners on the overall performance of candidates and individual questions as a guide for applicants for future sittings. These are available here.
Understand the SBA format and how to approach questions: this document also provides questions that have been used previously in the Final FRCR (Part A) Examination. You can find this here.
TNM Staging guidance - this document explains the knowledge required to answer questions related to this topic, available here.
Demonstration films: demonstrations of both parts of FRCR Part 2, providing insight into both elements of the exam and what candidates can expect on the day. These are on the RCR website here.
Scoring system for Part 2B: key information on how each part of the exam is marked, found here.
Courses
There are several online courses which provide preparation for the exams, including mock exams and insight into exam technique. As with all courses, we advise that you register your interest as soon as possible to avoid disappointment as they are in very high demand.
Please note these courses are subject to change and candidates are advised to book early (up to one year in advance in some cases), as spaces are often limited. Places may become available at the last minute, so make sure you add your name to a waiting list if possible.
Midlands FRCR 2A Review Course
This is an in-person revision course for the FRCR Part 2A exam held in Leicester. The course provides a refresher course covering a range of important topics, an interactive lecture-based course delivered in a ‘single best answer format’ and tips and tricks from trainees with recent experience of the exam.
Duration - 3 days
Cost - £350
London Heathrow FRCR 2B Preparation Course
This is a two-day course aimed at clinical trainees who are preparing for their FRCR CR2B. The course offers a minimum of 4 viva sets, 4 long case sets along with 4 rapid reporting packets. A further 2 lectures would also be included during the 2 days.
The course is delivered live virtually.
Duration - 2 days
Cost - £500
Red Dot Radiology Courses
These are in-person revision courses for Part 2B which cover rapid reporting as well as focused days on chest x-rays. The courses are live online via an interactive video and are led by FRCR qualified UK-based radiologists.
Duration - 1 day
Cost - £165
Aunt Minnie Courses
This is an online two-day course that runs twice a year and concentrates on Aunt Minnie cases that you may encounter in your FRCR 2B exam. The course is split into mini tests, workshops and exam tips to ensure candidates remain refreshed and stimulated.
Duration - 2 days
Cost - £350
Books
FRCR CR2A
Grainger & Allison’s Diagnostic Radiology
Fundamentals of Diagnostic Radiology - Brant & Helms
Primer of Diagnostic Imaging - Weissleder
Radiology Review Manual - Wolfgang Dahnert
Crack the Core Exam – Prometheus Lionhart
Fundamentals of Skeletal Radiology – Clyde A. Helms
Get Through Final FRCR 2A: SBAs - Teck Yew Chin, Susan Cheng Shelmerdine
RSBAs for the FRCR Part 2A - Richard Lindsay
FRCR CR2B
Rapid Review of Radiology - Shahid Hussain, Sherif Latif, Adrian Hall
Top 3 Differentials in Radiology - William O'Brien
Long Cases for the Final FRCR 2B - Rebecca Hanlon
Aunt Minnie's Atlas and Imaging-specific Diagnosis - Thomas Pope
Final FRCR Part B Viva: 100 Cases - Richard White, Robin Proctor, Ian Zealley
Chapman & Nakielny's Aids to Radiological Differential Diagnosis – Stephen Davies
#IMG Tips
Familiarise yourself with the exam content – the best way to do this is through the syllabus and curriculum
Prepare early – the earlier you begin your revision, the more structured and relaxed the entire process can be and the more likely you are to pass!
Invest in the right resources and courses – many resources from books to courses come at a cost – think about your own preferred style of learning and choose the resources that best suit you! Have any colleagues going through the exams or already passed? See if you can borrow or split the cost of resources.
Practise, practise, practise – this is of course a given...practise makes perfect and getting used to the format and being able to go through many sample questions will set you up well for the exam!
Sources
https://www.rcr.ac.uk/clinical-radiology/examinations/frcr-part-2a-radiology-cr2a
https://www.rcr.ac.uk/clinical-radiology/examinations/frcr-part-2b-radiology-cr2b
https://www.rcr.ac.uk/sites/default/files/clinical_radiology_curriculum_2020.pdf
Getting started
We hope this is helpful for any overseas doctors preparing to sit their Final FRCR exam and the team here at IMG Connect wish you the best of luck!
Follow us on social media through the links below for regular news and updates on the Royal College, relocating to the UK and working in the NHS.

BNO Visa vs Tier 2 Visa – a guide for Hong Kong doctors
Once you have received a job offer to work in the NHS, Hong Kong doctors have two options to choose from when applying for a visa: the British National Overseas (BNO) visa or the Tier 2 Skilled Worker visa for health and care workers.
The two visas have different criteria, requirements and merits, and which is best for any doctor will depend on the individual’s circumstances.
To help you better understand which visa is best suited to Hong Kong doctors relocating to the UK, we’ve put together this blog which will touch on the following questions:
What is a BNO Visa?
What is a Tier 2 Health & Care Worker Visa?
What are the differences between the two visas?
Which visa is better for me as a Hong Kong doctor?
I am relocating with family, which visa do they need?
What is the application process for the BNO visa?
What is the application process for the Tier 2 Health & Care Worker Visa?
#IMG Tips
I have completed my visa application, what’s next?
Skip ahead to the relevant section if you know what you’re looking for.
British National (Overseas) Visa
If you’re from Hong Kong and are a British national (overseas), you and your family members can apply for a British National (Overseas) visa, also known as a BNO visa. It allows you to live, work and study in the UK and was launched by the UK Home Office in 2021.
Within the BNO visa, there are two broad ‘routes’ which have the same general conditions but cater to two different groups of people:
BNO Status Holder route – for BNOs and their dependent partners or minor children. Other adult family members with a high degree of dependency may also apply under this route.
BNO Household Member route – for BNO citizens’ adult children (born on or after 1 July 1997) and the adult child’s dependent partner and minor children. All applicants must form part of the same household as the BNO citizen (i.e. normally live together) and be applying alongside the BNO family member.
Tier 2 Skilled Worker Visa (Health & Care)
A Tier 2 visa is what allows overseas health and care workers to live, and work in the UK. Similarly to the BNO visa, it is provided by the Home Office following a job offer from a UK employer with a valid Tier 2 Sponsorship License.
The list of valid Tier 2 Sponsors can be found here.
It is safe to assume that the NHS trust you are applying to has a valid Tier 2 Sponsorship licence and that your IMG Consultant will have already checked this for you.
The Tier 2 visa allows you to work in the UK for the duration of your sponsorship period.
You can also bring over certain family members with you on a Tier 2 Dependent visa.
For a detailed overview of the Tier 2 Health & Care Worker Visa, see our blog here.
BNO Visa vs Tier 2 Visa
The BNO or Tier 2 visa essentially serve the same purpose for Hong Kong doctors, but they have some differences and similarities which are important to understand in order to make an informed decision between the two.
The main characteristics of the two visas are summarised below:
Immigration Health Surcharge (IHS)
Some of the most significant differences between the two visas is that on the BNO visa, you and your dependents must pay the IHS, whereas the IHS is no longer applicable to doctors on the Tier 2 visa.
You can claim this back every 6 months, but processing can take up to 6 weeks, and you may be doing this several times throughout the duration of your visa. You can read more about this here.
Police Check or Certificate of No Criminal Convictions (CNCC)
For the Tier 2 visa, you are required to produce a CNCC by the Home Office, whereas it is not required for the BNO visa, but it is very likely that you will be asked by the Trust to provide one.
Certificate of Sponsorship (CoS)
On the Tier 2 visa, you will require a CoS, which is a digital reference number from a Certified Sponsor (your NHS Trust) which you will need to complete your visa application.
With the BNO visa, you do not need a CoS because this visa isn’t dependent on a job offer.
Dependents
The criteria for dependents are stricter with the Tier 2 visa than the BNO visa.
On the Tier 2 visa, the only people defined as dependents are your partner, children under 18 and children over 18 if they’re currently in the UK as your dependent, whereas the BNO visa has greater allowances for children over 18 and family members dependent on you because of illness, disability or age.
BNO or Tier 2 Visa for HK Doctors
Whether the BNO or Tier 2 visa is better is entirely dependent on the particular circumstances of each doctor, but options are entirely suitable for doctors relocating from Hong Kong to the UK.
As mentioned above, some of these deciding factors may be the eligibility criteria, any dependents you may have, or your rights once you are in the UK on that visa.
We know that securing a BNO visa in Hong Kong can be quite a challenge at present, so if you think that the Health & Care Visa is a more feasible or easier option for you, don’t hesitate to connect with us to discuss your options.
Visas for Families
If you are relocating to the UK with family, each member of your family will need to apply for a visa alongside you.
BNO Visa
For doctors travelling on the BNO visa, you will be able to have your family apply as ‘dependents’.
This can include your:
husband, wife, civil partner or unmarried partner
child or grandchild under 18
child 18 or older, born on or after 1 July 1997 (and their partner or child under 18)
parent, grandparent, brother, sister, son or daughter (18 or older) if they live with you and they’re dependent on you because of illness, disability or their age
When you apply, you will need to provide evidence of your relationship with these family members and that you normally live together.
As a British national (overseas), you’ll need to submit your application first to get an application number. This is called a Global Web Form (GWF) or a Unique Application Number (UAN). Your family members must use your application number when they apply.
Your family members will need to apply for a BNO visa with the same duration as yours (i.e. 2 years and 6 months or 5 years) and will be able to extend their visa if you apply to extend yours.
Adult dependent relatives will need to use your extension reference number, whilst other family members can apply separately from you.
The cost of your family’s BNO visa will be the same as yours - £180 or £250 (per person).
Tier 2 Visa
For doctors with a Tier 2 visa, your family will need a dependent visa to live with you in the UK. They will need to complete separate applications.
Your family members can apply for a dependent visa if they are your:
husband, wife, civil partner or unmarried partner
child under 18 (including if they were born in the UK during your stay)
child over 18 if they’re currently in the UK as your dependent
When you apply, you will need to provide evidence of your relationship with these family members and that you normally live together.
There can be a range of factors that will affect a family member’s eligibility for the Dependent visa, so we recommend you check here for full details.
Each family member will need to complete a separate application and pay the visa fee.
Once you have completed your own application for the Tier 2 visa, they’ll also will need your application number - you’ll get this when you apply. This number is called a Global Web Form (GWF) or a Unique Application Number (UAN). You’ll find it on emails and letters from the Home Office about your application.
As part of their application, your partner and children will need to prove their identity.
The cost of your family’s Dependent visa will be the same as yours – either £232 or £464 (per person).
BNO Visa Application Process
It is important to check what documents you will need before you begin your application.
As part of your online application, you’ll need to prove your identity. How you do this depends on what type of passport you have. You’ll either:
BNO visa applications can be completed from within the UK or outside the UK, but in either instance, the application is completed online, and the process is as follows:
Compile your details and scan all required documents before starting. You can find the full list of required documents here.
Start the application
Create a UK Visas and Immigration account
Pay the visa fee
Further actions will be prompted:
Download document check list - A helpful checklist to ensure you submit everything that is needed (we strongly recommend you use this to ensure nothing is missed).
Provide documents and biometric details - At this stage, you will need to download the UK Immigration: ID Check app to scan your passport with a biometric chip and upload a photo of yourself*. You can choose this option if you have a British National (Overseas) passport, a Hong Kong Special Administrative Region passport or a passport from an EEA country.
Making an appointment with your local visa application centre – If you do not hold a passport with a biometric chip, you can go to an appointment at a visa application centre to give your fingerprints and a photo - this is to get a biometric residence permit (BRP).
Selecting location for BRP pick up in UK – If you have applied for a BRP, you will have 30 days from your date of arrival in the UK to retrieve this from a post office, so think carefully about the location you choose in the UK. Once you’ve chosen, you will be sent a BRP collection letter which you should print and take to the post office to retrieve your BRP.
Submit your completed application
*If you choose not to apply for a BRP and your visa application is approved, you will be given a link to generate a code to share when necessary. This may be people concerned with your relocation such as your employer or landlord, and they will be able to use the code to check your status on the gov.uk website.
You can find the online application form here and you’ll be told what you need to do when you apply. Your IMG Consultant will also be able to assist you with the application.
Application Review
Once you’ve applied, you can expect to receive a decision within 12 weeks, though your application may take longer to process if you need to provide more evidence.
Please note, you can apply for the BNO visa from overseas, but you should wait for a decision on your application before you travel to the UK.
Tier 2 (Skilled Worker) Visa Application Process
Like the BNO visa, we always advise that you check what documents you will need before you begin your application.
Once you have accepted a job offer and pre-employment checks are complete, the hospital will apply for a CoS from the UK Home Office.
Health and Care Visa applications are complete online, and the process is as follows:
Compile your details and scan all required documents before starting. You can find the full list of required documents here.
Start and complete the application - Once you have entered all your details, the application service will offer an appointment at a local visa appointment centre near you.
Pay the visa fee
Further actions will be prompted:
Download document check list - A helpful checklist to ensure you submit everything that is needed (we strongly recommend you use this to ensure nothing is missed).
Provide documents and biometric details - At this stage, you can upload electronic copies of your documents.
Making an appointment with your local visa application centre - Once you have made an appointment you will receive your appointment confirmation letter via email. Make note of the details and print this confirmation to take with you to the appointment.
Selecting location for Biometric Residence Permit (BRP) pick up in UK - You will have 30 days from your date of arrival in the UK to retrieve your BRP from a post office, so think carefully about the location you choose in the UK. Once you’ve chosen, you will be sent a BRP collection letter which you should print and take to the post office to retrieve your BRP.
Submit your completed application
Application Review
Once you’ve completed all the above steps your application will be processed for review, and you’ll usually get a decision on your visa within:
4 weeks, if you’re outside the UK
8 weeks, if you’re inside the UK
Every application is different however, so your application may take longer to process if you need to provide more evidence.
You may be able to pay to get a faster decision. How you do this depends on whether you’re outside the UK or inside the UK.
#IMG Tips
Take time to choose best visa for you – speak to your IMG Consultant to discuss your options and circumstances to decide the best visa for you.
Gather and scan all documents early – go through the relevant checklist and read the guidance provided to stay on top of your application and minimise any delays
Think about the start date you want written on your CoS – if you will be applying for the Skilled Worker visa, think carefully about what date you want written on your CoS (it is only valid for 90 days)
Have your application checked before submitting – your IMG Consultant will be more than happy to double check your visa application before it’s submitted – take advantage, we’re here to help!
Apply for the CNCC early – you will almost certainly need a CNCC regardless of which visa you choose, so apply for this early to speed up the process.
My visa application is complete, what’s next?
First things first, congratulations! You are just a few steps away from completing your journey to the UK and can now firm up your relocation plans, putting into action your relocation checklist.
With your application under review, you should begin discussing your relocation plans with your IMG Consultant. This includes accommodation and travel, schooling, banking and any other questions you might have – our relocation team is happy to help!
Don’t forget, once your application is being processed, you can track its progress online.
Getting started
Don’t hesitate to get in touch using the buttons above (and below) to discuss job options in the NHS, from the typical doctor salary in the UK to the most suitable hospital locations for you.
If you have any other questions, please feel free to get in touch with our team.
For advice, guidance and news and updates for IMGs, join the conversation through the links below.
Sources
https://www.gov.uk/british-national-overseas-bno-visa
https://commonslibrary.parliament.uk/research-briefings/cbp-8939/
https://www.gov.uk/skilled-worker-visa
https://www.gov.uk/uk-family-visa
https://www.gov.uk/apply-immigration-health-surcharge-refund/healthcare-setting
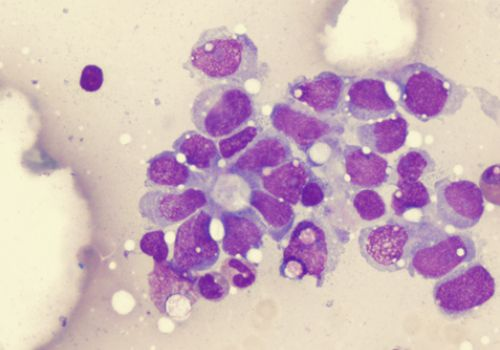
Where do I fit into the NHS with FRCR (Oncology)?
As there is no hard and fast rule for what position you will have after gaining a UK qualification, it is important for IMGs to understand the posts that are available to you after completing FRCR (Oncology).
FRCR (Oncology) is a highly beneficial qualification to achieve, but it does not guarantee you a consultant position in the NHS.
This can be a confusing area for overseas clinical and radiation oncologists, but this blog aims to de-mystify the subject. This article will explain the following topics:
What is FRCR (Oncology) and how does it fit into the UK training programme?
What grade will IMGs, new to the NHS, be offered with FRCR (Oncology)?
Can I take a permanent consultant post if I have FRCR (Oncology)?
CESR opportunities for clinical oncologists in the NHS
Skip ahead to the relevant section if you know what you’re looking for.
FRCR (Oncology) within the UK Oncology Training Programme
Fellowship of the Royal College of Radiologists (Oncology) or FRCR (Oncology) is the postgraduate qualification awarded by the Royal College of Radiologists, the body responsible for the specialties of clinical oncology and clinical radiology throughout the UK.
FRCR (Oncology) is a three-part exam which is a necessary part of the training programme of clinical oncologists in the UK.
For trainees who have chosen to pursue clinical oncology, FRCR (Oncology) Part 1 or CO1 must be passed by the end of ST4.
Clinical oncology trainees will then sit Final FRCR (Oncology), also known as Part 2A and 2B or CO2A and CO2B, usually from ST6 to ST7.
These final exams are important in that they assess a trainee’s knowledge and skills related to the investigation of malignant disease and the care and management of patients with cancer.
Any UK-trained clinical oncologist applying for a CCT in order to work as a substantive consultant must have completed full FRCR (Oncology).
As shown above, UK trainees will also have completed MRCP (UK), although this is not required for overseas clinical oncologists.
Positions for Doctors new to the NHS with FRCR (Oncology)
As an IMG with full FRCR (Oncology), you will be eligible for consultant grade positions in the UK.
You are not guaranteed a consultant position, particularly if you do not have previous consultant position in your home country, but you will certainly be able to attain more senior positions in the NHS, such as a specialty doctor (SAS) or specialist grade.
Consultant positions are the most senior in the UK, and thus the highest paid position for doctors within the NHS pay system.
For further information on how NHS pay scales work for consultants, please see our detailed article here.
Of course, this is assuming that you have also completed the other necessary components to make you eligible for GMC registration.
Alongside your postgraduate qualification, you will need to have passed an English Language Test (either IELTS or OET).
Additionally, you must obtain a Certificate of Good Standing, and submit this to the GMC. Upon the receipt of these three components, you will receive full GMC registration.
Permanent Consultant Posts with FRCR (Oncology)
To take up a permanent consultant position in the NHS, you would need to have Specialist Registration. Specialist Registration (more specifically CESR for most overseas doctors) allows you to take up permanent or substantive consultant roles in the NHS.
The type of consultant position you would be eligible for with FRCR (Oncology) is a locum consultant post.
Firstly, we should clarify the meaning of the term ‘locum consultant’ in the UK. The NHS has two types of locums - Trust locums and Agency locums.
If you are an IMG with full registration, but you are not on the Specialist Register, you are only able to take on consultant positions as a trust locum, but no permanent positions.
Trust locums are hired on a fixed-term contract and are able to better acclimatize themselves to the NHS system, whilst receiving the support and guidance to work towards consultant positions and CESR.
Please note, you can only work as an agency locum if you have a British passport.
CESR Opportunities in the NHS
CESR or the Certificate of Eligibility for Specialist Registration is a route of entry to the Specialist Register for those doctors who have not followed a GMC-approved training programme.
You can read more about CESR in Clinical Oncology through our IMG Resources library here.
IMG Connect are able to help you to secure senior roles such as specialty doctor (SAS), specialist grade or locum consultant in Trusts that offer CESR support.
In these roles, you will have better pay and responsibilities that are more appropriate to your level of experience compared to a trainee. These Trusts have a lot of experience in supporting overseas doctors to progress their careers through CESR.
You can collect evidence of your competences, particularly those specific to the UK Clinical Oncology curriculum and those you may not be able to achieve outside the UK.
These positions also facilitate a faster route to the UK than applying directly through the CESR route, which can take a substantial amount of time.
Get in touch with us to find out more about senior positions in the NHS with CESR support.
Getting started
We hope this blog has been helpful in clarifying your questions about securing senior posts in the NHS with FRCR (Oncology). If you have any further questions regarding the postgraduate exams, CESR or Oncology in the NHS - feel free to contact us directly.
Join the IMG Oncologists Facebook group for access to a community of like-minded clinical and radiation oncologists and dedicated oncology recruiters.
In this group you will find tailored support for oncology IMGs, including access to our NHS and CESR webinars, completely free to all doctors.
You can access our IMG Oncologists community here.
Follow us on social media through the links below for regular news and updates on the Royal College, relocating to the UK and working in the NHS.

Specialty Doctor Posts in Psychiatry with CESR Support
NHS Hospitals across the UK are offering specialty doctor job plans in Psychiatry with the opportunity for programmed CESR support, giving psychiatrists the chance to quickly work towards Specialist Registration.
For experienced IMGs, this is a new and relatively quick route to your first consultant post in Psychiatry.
By taking up a service level job as an SAS Doctor with CESR support as part of the job plan, many overseas psychiatrists are securing a great start to their career in the NHS that is suited to their senior level experience, whilst taking the time to acclimatize to the NHS and their Trust.
CESR Programmes for Specialty Doctors
By taking such posts in the NHS, you can join diverse, dynamic and inspiring groups of specialty doctors and acting consultants all on the way to achieving Specialist Registration as part of a tailored programme. You can read more about CESR for psychiatrists here.
In offering such job opportunities, Trusts will provide a supportive environment with protected time to fulfill all the requirements of the CESR application in Psychiatry and its sub-specialties, gaining career-enhancing experiences as you do.
Acting up, dedicated peer groups, coaching & mentoring, scheduled learning and study time are some of the benefits that you could receive in one of these roles.
In such roles you will typically receive hands on support from consultant colleagues and exposure to a wide range of experience to specifically aid competency achievement for your CESR application in relation to the Specialty Specific Guidance (SSG) for your sub-specialty.
In some specialty doctor jobs with CESR programme you will rotate through various departments, dependent on your required experience.
Some Mental Health Trusts will also provide the following as part of their CESR programme:
A number of Supported Professional Activity (SPAs) sessions per week
Tailored experience to your CESR portfolio
Regular clinical supervision
A CESR mentor
Involvement in academic programmes and medical student teaching
Support in gaining research competencies
SAS Tutor support
CESR / SAS support forums and meetings
Finding SAS Roles with CESR Support
If you are an overseas doctor looking for a Specialty Doctor job with the chance to work towards your Certificate of Eligibility for Specialist Registration (CESR) in Psychiatry, speak to the IMG Connect team to discuss if this is a suitable route for you.
We have opportunities across the UK for international psychiatrists to take advantage of the CESR programme.
You can also send your CV to info@imgconnect.co.uk or register here. It takes less than 30 seconds to register!
IMG Jobs
Search and find live Psychiatry jobs in the NHS with CESR support
IMG Resources Library
Browse our library for more useful articles on NHS jobs in psychiatry, salaries for doctors in the UK and postgraduate qualifications for psychiatrists and much more!
Connect with us
Don’t hesitate to get in touch using the buttons above (and below) and chat with an IMG Consultant to discuss your options for NHS roles with CESR support and start your journey towards Specialist Registration with IMG Connect.
For access to a community of like-minded psychiatry IMGs and dedicated psychiatry recruiters, join the IMG Psychiatrists Facebook group.
To receive the latest news and updates on all things psychiatry, including the Royal College, GMC registration and the NHS, follow us on social media and join the conversation.